 Shoulder & Elbow Service Fellowships
Shoulder & Elbow Service Fellowships
Interview Packet 2027-2028
Download PDF
Why is Seattle a great place to live and work?
Our Fellowship Faculty
Each faculty member has an international reputation as a shoulder surgeon, each provides the fellow with a unique approach to the evaluation and management of shoulder conditions.
Click on the names below for their backgrounds and interests.
Frederick A. Matsen III, M.D.
Matsen@uw.eduRick Matsen as been doing and teaching shoulder surgery at the University of Washington since 1975, after a fellowship with Dr. Charles Neer. He is the holder of the Douglas T. Harryman Jr / DePuy Endowed Chair for Shoulder Research, named in honor of our first shoulder fellow and late faculty member Doug Harryman. Funds from this Chair support an active research program, enabling our fellows to conduct cutting edge research. Rick continues an active practice with a focus on the evaluation and management of patients with cuff disorders, glenohumeral arthritis and failed arthroplasty. He enjoys teaching the principles and practice of shoulder surgery to our fellows as well as partnering with them in ongoing research. He frequently blogs on hot topics in shoulder surgery; shoulderarthritis.blogspot.com has over 2600 posts with over 1.8 million page views from over 100 countries. He has published over 250 peer-reviewed papers, many with our shoulder fellows. He looks forward to continuing his practice, research and teaching for years to come.
Albert O. Gee, M.D.
ag112@uw.eduDr. Albert Gee is an Associate Professor and a Vice Chair in the Department of Orthopaedics at the University of Washington. He specializes in Shoulder and Elbow as well as Sports Medicine surgery and is the Chief of the Sports Medicine Service. Dr. Gee came to UW after completing residency training at the University of Pennsylvania and a fellowship in Sports Medicine and Shoulder surgery at the Hospital for Special Surgery. He cares for patients with a variety of shoulder, elbow and knee conditions and his clinical focus is in arthroscopic treatment of shoulder and knee injuries. In addition to his practice at the UW, he also cares for Veterans at the Puget Sound VA Health System and he serves as a Team Physician for the University of Washington Huskies. Dr. Gee has a broad range of research interests from basic science to clinical outcomes and athlete injury prevention. List of recent publications can be seen here.
Jason E. Hsu, M.D.
jehsu@uw.eduDr. Jason Hsu is an Associate Professor in the Department of Orthopaedics and Sports Medicine and is the Program Director of the Shoulder and Elbow Fellowship. Dr. Hsu joined the faculty at the University of Washington in 2014 after completing residency at the University of Pennsylvania and shoulder and elbow fellowship at Washington University in Saint Louis. He maintains a busy practice of both open and arthroscopic shoulder and elbow procedures, from straightforward arthroscopic Bankart repairs, cuff repairs, and primary shoulder arthroplasty to complex revision reconstructions of multiply-failed shoulder arthroplasties. He is currently holder of the Rick and Anne Matsen Honorary Professorship for Shoulder Research and has research interests focusing primarily on the role of Cutibacterium in failed shoulder arthroplasty and predictors of success for both primary and revision shoulder arthroplasty. List of recent publications can be seen here.
Corey Schiffman, M.D. Corey Schiffman, MD, is an orthopaedic surgeon specializing in shoulder and elbow surgery. Dr. Schiffman believes in a team approach to patient care and utilizes the practice of evidence-based medicine to offer his patients leading-edge surgical techniques and procedures. His main goals are improving quality of life and helping patients return to the most enjoyable activities. Dr. Schiffman's clinical expertise includes the arthroscopic and open treatment of all shoulder and elbow conditions, including arthritis, tendon disorders, joint instability, and fractures. Common procedures include shoulder and elbow replacement, arthroscopic rotator cuff repair, arthroscopic shoulder stabilization, tendon transfers, fracture fixation, and sternoclavicular joint reconstruction. List of recent publications can be seen here.
Our Fellowship Coordinator: Fred Westerberg (fwesterb@uw.edu)
Address:
University of Washington Medical Center
Department of Orthopaedics and Sports Medicine
1959 NE Pacific Street, Box 356500
Seattle, WA 98195-6500
Phone: (206) 543-3690 Fax: (206) 685-3139
Stipend: $87,724/year plus benefits
Number of fellows per year: Two
More Information on our fellowship:
A broad and deep surgical experience with a vast spectrum of disease processes including arthritis, instability, cuff disease, fractures, sports as well as acromioclavicular, sternoclavicular and scapulothoracic conditions, each approached with rigor and resultant individuality. Commonly an individual fellow performs an anatomic total shoulder, a ream and run procedure, a reverse total shoulder, a cuff tear arthropathy arthroplasty, a revision arthroplasty and a humerus ORIF in a single week. The faculty are dedicated to providing a robust “hands on” experience for each fellow.
Blog with the latest information on shoulder arthritis and rotator cuff disease:: http://shoulderarthritis.blogspot.com
Stimulated by a 5-month experience that Dr. Matsen had with Dr. Charles Neer – the father of American Shoulder Surgery – the UW Department of Orthopaedics and Sports Medicine decided to offer an advanced experience to selected individuals interested in advanced training in shoulder and elbow. Beginning in 1988, this was one of the first one-year shoulder fellowships in the world.

Our first fellow was the late Douglas T. Harryman II, who made many enduring contributions to the understanding of surgical approaches and the mechanics of the shoulder. He was also a pioneer in arthroscopic approaches to rotator cuff disease, instability, and the management of the stiff shoulder.

Decades later, the goal of our fellowship remains the same - to provide a cutting edge clinical and academic experience to the shoulder and elbow surgeons of the future.
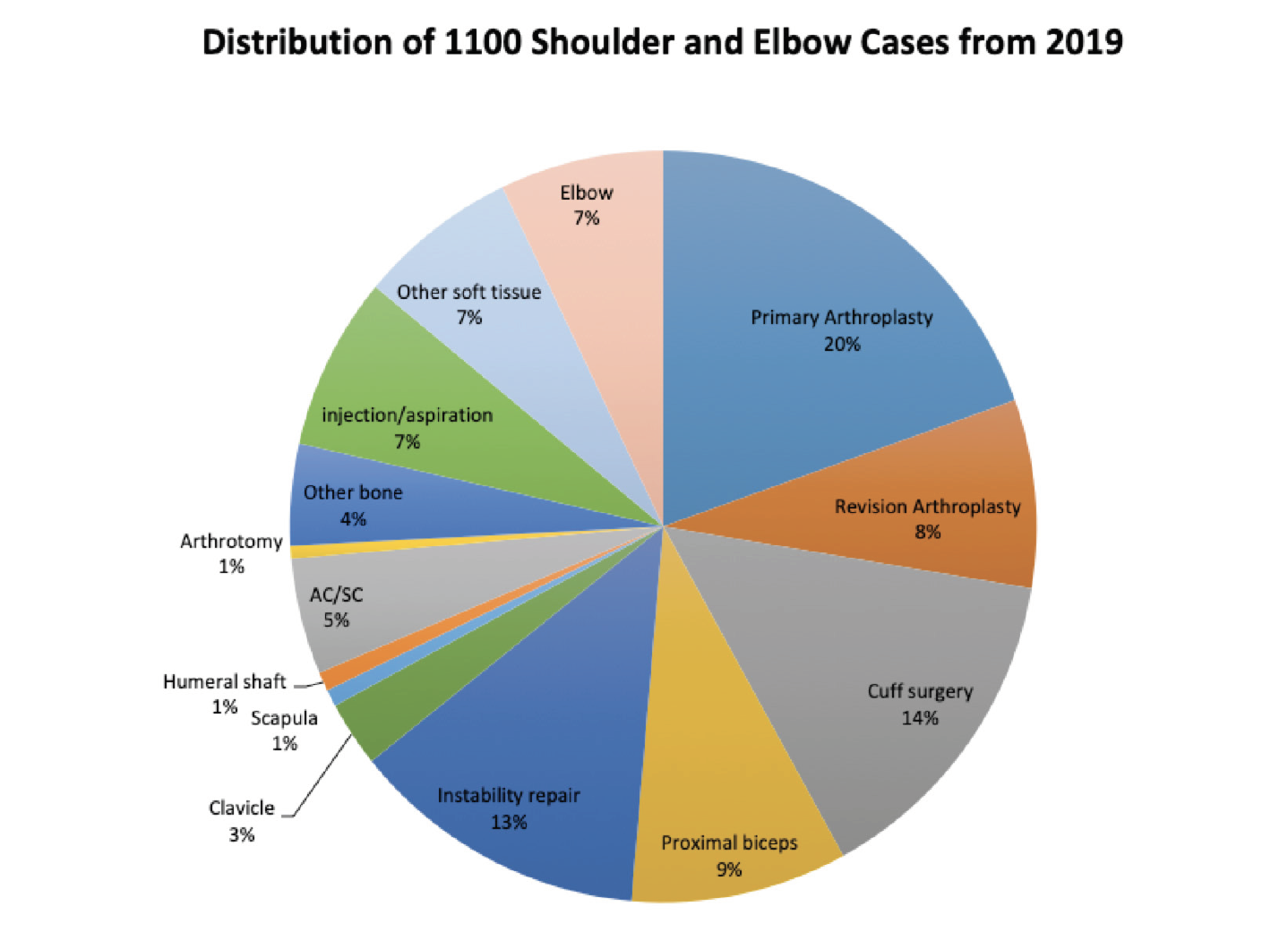
Our service provides a broad clinical experience, with approximately 1,000 shoulder and elbow surgeries per year of which 39% are arthroscopic procedures, 28% are arthroplasties, 11% are for fractures, and 17% are for a variety of other problems, ranging from management of acromioclavicular and sternoclavicular joint problems to pectoralis major transfers. Our Fellows learn not only how to perform the most effective, evidence-based surgical procedures, but also how to think about and manage each individual patient. Our weekly experience includes clinic, pre-op conference, the operating room, post-op conference, and research. Cadaver and dry laboratories are held to allow the Fellows to practice arthroscopic and open reconstructive procedures in a quality laboratory setting.
Our weekly experience includes clinic, pre-op conference, the operating room, post-op conference, and research.
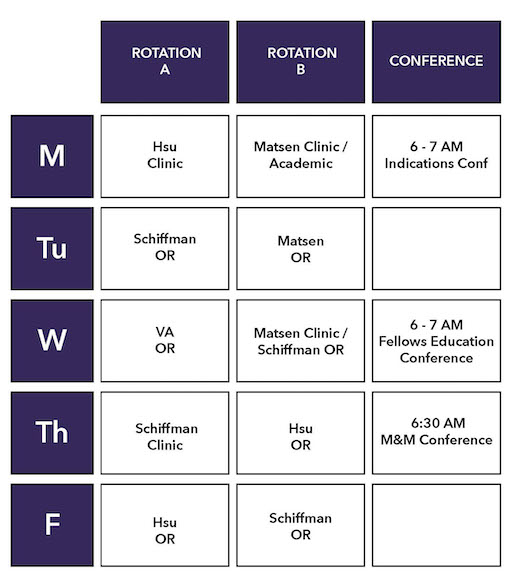
- BJC (Bone and Joint Center) is our main clinic also known as Hand, Elbow & Shoulder Center at UWMC Roosevelt.
- Pavilion is the UWMC Surgery Pavilion located at University of Washington Medical Center.
- Northwest is Northwest Hospital, now part of the University of Washington Medical Center, located in North Seattle.
- ESC is the Eastside Specialty Center located in Bellevue, WA.
Cadaver and dry laboratories are held to allow the fellows the opportunity to practice arthroscopic and open reconstructive procedures in a quality laboratory setting.
Our research program is securely supported by the Douglas T. Harryman / DePuy Endowed Chair for Shoulder Research and the Rick and Anne Matsen Endowed Professorship for Shoulder Research. Our assets include a long-standing and data-rich arthroplasty database and two research coordinators.
Fellows are expected to complete several research projects during the year and to submit their findings for publication to orthopaedic peer-reviewed journals.
Our investigative interests currently focus on:
- identifying the predictors of good and poor results for surgical procedures,
- analyzing failures of surgery with an eye to prevention,
- continuing to explore the difficult problem of Cutibacterium in failed shoulder surgery, and
- challenging the 'conventional wisdom' when it is unsupported by evidence.
Qualified applicants must have completed a certified residency program in orthopaedics at the time the fellowship is started and should have a strong commitment to academic orthopaedics. Interested candidates should send a curriculum vita, a personal statement that includes professional plans and goals, and four letters of recommendation. From those applying we invite the most competitive candidates for interviews conducted between January 4, 2026 and April 6, 2026. Candidates will be matched through the ASES Fellow selection process. The University of Washington is an equal opportunity affirmative action employer.
The Growing Legacy of our Shoulder and Elbow Fellowship
The UW Shoulder and Elbow Fellowship has trained over 61 outstanding shoulder and elbow surgeons over the past 37 years. Their names and contact information are listed in the Shoulder & Elbow Fellowship Alumni tab. Many are now leaders in shoulder and elbow surgery. Over half of our fellowship graduates have earned membership in the American Shoulder and Elbow Surgeons; a select group that Dr. Matsen helped found along with Drs. Hawkins, Cofield, Warren, Rockwood as well as Dr Neer in 1982.
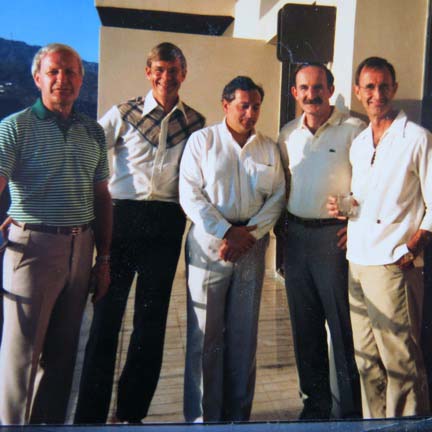
Our graduate fellowship ASES members include Mark Lazarus at Rothman, Richard Boorman at the University of Calgary, Ryan Bicknell at Queen’s University, Ben Goldberg at University of Illinois, Matt Saltzman at Northwestern, Michael Pearl at Kaiser, Yong-Girl Rhee at the Kyung Hee University School of Medicine, Seoul and Tony Romeo at Rush; Tony is the incoming President of the American Shoulder and Elbow Surgeons (middle of back row among a group of early fellows at a reunion).

Our most recent fellow to join ASES is Joe Lynch who was granted membership this year.
The legacy of the fellowship also includes well over 250 publications in premier orthopaedic journals and several texts, including Rockwood and Matsen’s The Shoulder, which is nearing publication of its 6th Edition with Dr. Matsen as the senior editor. The sixth edition will have its debut at the coming annual meeting of the AAOS in 2020.
These publications would not have been possible without the substantial contributions and authorship of our fellows. Again this year our fellows are actively involved in research that will permanently change the evaluation and management of patients with shoulder and elbow problems.
The legacy of our fellowship includes foundational concepts that have been developed here at the University of Washington by Drs. Warme, Hsu, Gee, Matsen and our fellows.
Some of these foundational concepts are listed below.
Treatment outcomes
- The key to evaluating the outcome of surgery is a quick, sensitive, validated tool by which the patient can document the status of his/her shoulder before and sequentially after treatment without having to return to the office = the Simple Shoulder Test. This simple metric that we introduced in the mid 1990’s has been used in over 200 publications and in multiple languages around the world. It has become the benchmark for cost-effective patient-reported documentation of the shoulder’s comfort and function.
- The result of a treatment is determined by the 4 Ps: the characteristics of the patient, the shoulder problem being treated, the procedure used to treat the problem, and the physician rendering the treatment for the patient.
- The value of an evaluation and management approach can be defined as the benefit to the patient divided by its cost. For example if a preoperative CT scan of an arthritic shoulder does not lead to an improved outcome for the patient, it is of less value than less expensive and less irradiating plain films. We use the concept of value to examine new technologies, such as patient-specific instrumentation, platform prostheses, and augmented glenoid components.
Glenohumeral stability
- The primary stabilizing mechanism for the shoulder is concavity compression – the compressive action of the cuff and deltoid forces centering the humeral head in the glenoid concavity throughout the range of motion, including the many positions in which the ligaments are lax. Treatment of instability requires restoration of this mechanism.
- An anatomic repair of the Bankart lesion is sufficient for the management of most cases of recurrent glenohumeral instability. Bone transfers, such as the Latarjet procedure or iliac crest graft, have increased complication rates and morbidity – for those reasons they are reserved for cases of failed anatomic repairs or cases of massive glenoid bone deficiency.
- Pain pump infusion of local anesthetics is not necessary in the management of glenohumeral instability and can lead to the complication of chondrolysis.
Sternoclavicular joint
- The unstable SC joint can be safely reconstructed by an allograft weave.
Rotator cuff
- An intact supraspinatus is not necessary to initiate abduction.
- The outer aspect of the proximal humeral convexity normally contacts and articulates with the concavity of the coracoacromial arch, providing stability resisting superiorly directed forces. This contact is not ‘impingement’. Sacrifice of the CA arch by acromioplasty can lead to anterosuperior escape and pseudoparalysis. The cuff muscles are not ‘head depressors’, but rather ‘head compressors’.
- In patients with a symptomatic irreparable cuff tear and an intact coracoacromial arch, comfort and function can often be improved by a smooth and move procedure that removes roughness from the proximal humeral convexity and restores full passive range of motion without attempting a cuff repair or graft.
- Acromioplasty is unnecessary in the treatment of cuff disease.
- Recent ‘advances’ in rotator cuff repair techniques have not led to improved clinical results or to reduced rates of retear. The integrity of the cuff repair is not strongly related to the clinical outcome of the surgery.
Arthritis
- CT scans are unnecessary in the evaluation of most cases of glenohumeral arthritis. The key image is the ‘truth view’ – a standardized axillary view taken with the arm in a position of functional elevation. This view shows the glenoid version, the glenoid type, and the degree of posterior functional decentering of the humeral head on the glenoid.
- Lesser tuberosity osteotomy is not necessary to gain access to the glenoid or to achieve restoration of subscapularis integrity. LTO has the disadvantage of compromising the ability to get a secure proximal press fit of the stem with impaction grafting.
- Metal-backed glenoid components have a higher failure rate than all polyethylene pegged glenoid components.
- ”Correction” of glenoid retroversion is not a priority in shoulder arthroplasty; posterior decentering can be effectively managed by an anteriorly eccentric humeral head component and rotator interval plication.
- Avoiding the use of a guide wire enables the surgeon to ream the glenoid to a single concavity with the removal of a minimal amount of bone. 3D planning based on CT scans and patient specific instrumentation add cost and radiation without documented benefit to the patient.
- Bone ingrowth, porous coating, and trabecular metal are unnecessary for the fixation of the humeral component; robust, bone-conserving and durable fixation of the prosthesis can be reliably achieved by impaction autografting using bone harvested from the resected humeral head.
- Impaction grafting facilitates the intra-operative adjustment of the height, version, and angle of the humeral prosthesis by selective addition and positioning of the graft.
- The use of small diameter humeral stems along with impaction grafting avoids the stress riser at the tip of the prosthesis and avoids the risk of incomplete seating of the humeral stem due to incarceration of the prosthetic tip in the diaphysis.
- Fixation of the humeral stem with impaction grafting greatly facilitates revision should that become necessary, eliminating the need to remove cement and minimizing the risk of fracture and the need for humeral osteotomy.
- Excellent functional restoration for the arthritic shoulder can be achieved without the use of a prosthetic glenoid component. The ream and run procedure provides a non-prosthetic approach to glenoid arthroplasty, avoiding the potential risks associated with plastic and bone cement.
Cuff tear arthropathy
- In patients with active elevation above 90 degrees and without anterosuperior escape, comfort and function can be improved using a CTA prosthesis that may be a preferable option (in comparison to a reverse total shoulder) for patients desiring heavy physical use of the shoulder or those who have a high fall risk.
Reverse total shoulder
- Prostheses that enable immediate robust glenoid fixation with a large central screw and lateralization of the glenosphere provide secure glenohumeral stability and minimize the risk of scapular notching and polyethylene failure.
- If the tuberosities are intact, secure humeral component fixation can be achieved with impaction autografting of a monoblock stem.
Periprosthetic infections
- Cutibacterium are normal inhabitants of the dermal sebaceous glands where they cannot be reached by epidermal skin preparation and from where they are released into the wound by skin incisions or by needles used for injection.
- Cutibacterium periprosthetic infections present in a “stealth” mode, rather than in the “obvious” mode characteristic of hip and knee periprosthetic infections.
- Cutibacterium are the most common organisms to be recovered from failed arthroplasties. They can only be reliably recovered if special culture techniques are used and if the cultures are observed for three weeks.
- Ceftriaxone and Vancomycin are preferred to Cephazolin or Clindamycin for preoperative prophylaxis due to the evolving sensitivity profile of Cutibacterium.
- A single-stage exchange to an impaction allografted hemiarthroplasty is usually sufficient for the management of a periprosthetic infection with Cutibacterium.
We hope this summary provides a useful view of our growing legacy. While we have made some substantial contributions to the foundation of knowledge on which shoulder surgery is practiced, there are many more opportunities ahead and we look forward to working with future fellows in uncovering them.
A few final comments: While we are a hard-working team, we have a good time working together and enjoying all the terrific opportunities the Seattle area has to offer.
The fellowship year ends with both a formal graduation
and an informal party generously hosted by Winston and Jeanne Warme.

We are very proud of what each of our graduates are accomplishing in their practices and treasure the role we have had in enabling their future.