Last updated: Wednesday, January 26, 2005
Eight clinical entities
The discussion of treatment will be divided in terms of eight clinical entities: asymptomatic cuff failure posterior capsular tightness subacromial abrasion failed acromioplasty partial thickness cuff lesions full thickness cuff tears failed cuff repair and cuff tear arthropathy.
Asymptomatic cuff failure
In this condition the shoulder does not bother the patient but imaging studies document a full thickness defect in the cuff tendon. (Harryman Mack 1991 Matsen Lippitt 1994 Milgrom Schaffler 1995 Pettersson 1942 Sher Uribe 1995)
Minimal symptoms
The realization that full thickness cuff tears may be asymptomatic poses substantial questions regarding the prevalence of cuff tears in the general population and the indications for rotator cuff surgery. It is difficult to improve patients who have minimal symptoms. The case for surgery to prevent future problems in such patients has not been convincingly made.
Posterior capsular tightness
In this condition the shoulder is limited in its range of internal rotation in abduction cross-body adduction internal rotation up the back and flexion (in approximate order of decreasing frequency).
Slightly frozen shoulder
The symptoms and physical examination of this "slightly frozen shoulder" may be similar to those described for the "impingement syndrome" (Cofield and Simonet 1984) including difficulties sleeping and reaching cross the body and up the back.
Posterior capsular tightness
The patient with posterior capsular tightness is informed that this condition is a common result of a mild injury to the rotator cuff but that in the absence of weakness or pain on isometric muscle testing non operative management is usually successful. The most effective program is one that taught by the surgeon or therapist but is carried out by the patient. The recommended treatment consists of gentle stretches performed five times a day by the patient (see figures 1-6). Each stretch is performed to the point where the patient feels a pull against the shoulder tightness but not to the point of pain. Each stretch is performed for one minute so that the patient invests about 30 minutes per day in their shoulder. Obvious improvement commonly occurs within the first month but three months may be required to completely eliminate the condition. The rare refractory case may be considered for an arthroscopic capsular release as described by Harryman. (Harryman Matsen 1996)
Subacromial abrasion
In subacromail abrasion without a significant defect in the cuff tendon the shoulder demonstrates symptomatic crepitus as the humerus is rotated beneath the acromion; isometric testing of the cuff muscles reveals no pain or weakness.
Nonoperative treatment
Patients in whom the primary complaint is symptomatic subacromial crepitance (see figure 7) will usually benefit from reassurance and a home program of gentle stretching and strengthening exercises. Various nonoperative rotator cuff programs have been described for the general population and for athletes including throwers. (Albright Jokl 1978 Atwater 1979 Berry Fernandes 1980 Binder Parr 1984 Cofield 1985 Cofield and Simonet 1984 Fowler 1979 Hawkins and Kennedy 1980 Jobe and Moynes 1982 Kerlan Jobe 1975 Neer 1983 Neviaser Neviaser 1982 Pappas Zawacki 1985a Pappas Zawacki 1985b Richardson Jobe 1980 Rocks 1979 Scheib 1990) Exercises must address specifically any shoulder stiffness which may cause obligate translation and loss of concentricity on shoulder movement (see figure 8). The effectiveness of nonoperative treatment was recognized many years ago by Neer who in his initial article on anterior acromioplasty pointed out that "Many patients . . . were suspected of having impingement but responded well to conservative treatment." (Neer 1972) Furthermore he stated that patients were advised not to have an acromioplasty until the stiffness of the shoulder had disappeared and the disability had persisted for at least nine months. As a result of these conservative surgical indications during the period covered by his report this most active shoulder surgeon operated on an average of only ten shoulders a year with this diagnosis: the effectiveness of nonoperative management is worthy of emphasis!
The low success rate in returning athletes to competition after acromioplasty (Tibone Jobe 1985) reinforces the importance of nonoperative management in this population. Similar principles apply to workers who are required to use their shoulders in positions aggravating subacromial abrasion.
Subacromial injections of corticosteroids have been reported by some to produce symptomatic relief. (Hollingworth Ellis 1983) However Withrington and coworkers (Withrington Girgis 1985) reported a double-blind trial of steroid injections and found no evidence of the efficacy of such treatment. Valtonen (Valtonen 1978) found no difference between subacromial and gluteal injections of steroids. Berry and colleagues (Berry Fernandes 1980) compared acupuncture physiotherapy steroid injections and anti-inflammatory medications and found no difference among these treatments.
Steroid injections in or near the cuff and biceps tendons may produce tendon atrophy or may reduce the ability of damaged tendon to repair itself. Such changes have been well documented in other tissues. (Lund Donde 1979 Rostron Orth 1979 Uitto Teir 1972) Uitto and colleagues (Uitto Teir 1972) demonstrated corticosteroid-induced inhibition of the biosynthesis of collagen in human skin. The harmful effects of repetitive intra-articular injection of steroids have been noted. (Behrens Shepherd 1975 Cruess Blennerhassett 1968 Mankin and Conger 1966 Salter Gross 1967 Sweetnam 1969)
Ford and DeBender (Ford and DeBender 1979) reported 13 patients who developed 15 ruptured tendons subsequent to nearby injection of steroids. Other authors have reported spontaneous ruptures of the Achilles tendon and patellar tendon after steroid injection. (Bedi and Ellis 1970 Ismail Balakishnan 1969 Lee 1957 Melmed 1965 Smaill 1961) Although Matthews and colleagues (Matthews Sonstegard 1974) failed to find a deleterious effect of corticosteroid injections on rabbit patellar tendons Kennedy and Willis (Kennedy and Willis 1976) found a substantial effect in the rabbit Achilles tendon. They concluded that physiological doses of local steroid placed directly in a normal tendon weaken it significantly for up to 14 days following the injection.
Watson (Watson 1985) reviewed the surgical findings in 89 patients with major ruptures of the cuff. He found that all 7 patients who had had no local steroid injections had strong residual cuff tissue. Thirteen of 62 patients having one to four steroid injections had soft cuff tissue that held suture poorly; 17 of the 20 patients having more than four steroid injections had very weak cuff tissue; these shoulders with weak cuff tissue had poorer results after surgical repair. In this light one can appreciate the potential hazard of making a diagnosis of "bursitis" or "bicipital tendinitis" and treating the situation with repeated steroid injections until the reality of a major cuff tendon deterioration becomes inescapable. (Darlington and Coomes 1977 Kennedy and Willis 1976)
The patient with subacromial abrasion is informed that this condition can usually be resolved with nonoperative management directed toward the restoration of normal mobility strength coordination and fitness.
Authors' preferred method of nonoperative management of subacromial abrasion
In our approach to subacromial abrasion we recognize the important interplay between cuff weakness stiffness of the posterior capsule and subacromial roughness. We use a program designed by Sarah Jackins a physical therapist who has worked with the University of Washington Shoulder and Elbow Service since its inception in 1975. This treatment regimen is analogous to one that would be used for managing a tennis elbow or Achilles tendinitis and includes:
- avoidance of repeated injury
- restoration of normal flexibility
- restoration of normal strength
- aerobic exercise and
- modification of work or sport.
The emphasis is on simple low-tech exercises that the patient can perform unassisted.
The Jackins Program
Step 1: Avoidance of Repeated Injury
Although it seems obvious that an affected shoulder must be rested we see patients each week who are trying to continue vigorous overhead work or swimming hundreds of miles per week in the presence of cuff symptoms. It is difficult to treat these symptoms when the affected area is repeatedly irritated; activities may need to be temporarily modified--light duty reducing mileage less throwing using the kickboard for a major part of the workout rather than continuing to try to "swim through" the problem or working on the forehand and footwork rather than beating away at the serve. Once symptoms have subsided the activity is progressively resumed with an emphasis on proper technique and a paced resumption of normal levels of performance.
Step 2: Restoration of Normal Flexibility
The goal of Step 2 is to stretch out all directions of tightness. Shoulders with subacromial abrasion are frequently stiff especially in the posterior capsule. As described above for posterior capsular tightness the most effective program is one that taught by the surgeon or therapist but is carried out by the patient. The goal of the flexibility program is to restore the range of motion to that of the unaffected shoulder. The recommended treatment consists of gentle stretches performed five times a day by the patient (see figures 9-14). Each stretch is performed to the point where the patient feels a pull against the shoulder tightness but not to the point of pain. Each stretch is performed for one minute so that the patient invests about 30 minutes per day in their shoulder. Obvious improvement commonly occurs within the first month but three months may be required to completely eliminate the condition.
Step 3: Restoration of Normal Strength
When near-normal passive flexibility of the shoulder is restored the patient's attention is directed toward regaining muscle strength. As is the case in managing tennis elbow it is most effective to delay strengthening exercises until normal range of motion is achieved. As with the flexibility exercises the patient is given the responsibility for strengthening the shoulder. Internal and external rotator-strengthening exercises are carried out with the arm at the side (see figures 15 and 16) to strengthen the anterior and posterior cuff muscles without the potential for subacromial grinding that exists with exercises in abduction and flexion. These exercises are most conveniently performed against the resistance of rubber tubing sheet rubber bike inner tubes springs or weights. It is convenient if the resistance device can be carried in a pocket or purse for frequent use through the day. As strength increases the patient is advanced to more resistance: thicker tubing tougher rubber sheets or more springs. Deltoid strengthening is added when it can be performed comfortably (see figure 17) as are exercises to strengthen the scapular motors (see figure 18). Athletes are not returned to full activity until the shoulder has full mobility and strength.
Step 4: Aerobic Exercise
If a patient has gotten out of shape as a result of the shoulder problem it is important to emphasize the need to regain normal fitness. To get back in shape and to improve the sense of well-being a half hour of "sweaty" exercise five days a week is recommended. Brisk walking may be the safest and most effective type of aerobic exercise but other suitable forms include jogging biking stationary biking and so on. Aerobic calisthenics as usually defined must be carefully reviewed to ensure that they do not require arm positions which aggravate the patient's symptoms.
Step 5: Modification of Work or Sport
Obviously the purpose of the program is to return the patient to the comfortable pursuit of normal activities. Not infrequently this requires some analysis of working and recreational techniques. Occasionally this is as simple as having the short grocery clerk stand on a platform at work. The technique of swimmers is reviewed to ensure for example adequate roll on the freestyle stroke. Throwers are taught the importance of body position and rotator cuff strength. Adequate knee bend and lumbar extension is reinforced in the execution of the tennis serve. If the patient has an occupation that requires vigorous or repeated use of the shoulder in painful positions vocational rehabilitation to a different job may be required.
Subsequent Steps
It may take six weeks before substantial benefit is realized. As long as the patient is making progress we continue this program. If improvement is not forthcoming the program is reviewed to be sure it is being conducted in an ideal way. The shoulder and the patient are also reevaluated to make sure there are no other factors that may be interfering with recovery. If repeat clinical evaluation indicates positive tendon signs (see figure 19) or other evidence of cuff fiber failure tendon imaging studies may be considered if their results would change the patient's management. If a well-motivated patient continues to have symptomatic subacromial abrasion after six months of a well-conducted program subacromial smoothing may be discussed as an alternative to continued non-operative management. Poor compliance with an exercise program may foretell an equally poor result from surgical treatment.
Operative treatment
Open acromioplasty
In his classic description of acromioplasty Neer (Neer 1972) described approaching the shoulder through a 9 cm incision made in Langer's lines from the anterior edge of the acromion to a point just lateral to the coracoid. The deltoid is split for 5 cm distal to the acromioclavicular joint in the direction of its fibers. It is then dissected from the front of the acromion and the acromioclavicular joint capsule. The stump of the deltoid's tendinous origin is elevated upward and preserved for the deltoid repair. Using an osteotome a wedge-shaped piece of bone .09 cm by 2.0 cm is resected from the anterior undersurface of the acromion along with the entire attachment of the coracoacromial ligament. If acromioclavicular osteophytes are present the distal 2.5 cm of the clavicle are also excised along with the prominences on the acromial side of the joint. After the procedure the deltoid is carefully repaired to the acromioclavicular joint capsule the trapezius and its tendon of origin.
Many reports regarding the results of open acromioplasty have been published. (Armstrong 1949 Diamond 1964 Ha'eri Orth 1982 Hammond 1962 Hammond 1971 Hawkins and Kennedy 1980 Jackson 1976 Kessel and Watson 1977 McLaughlin 1944 Michelsson and Bakalim 1977 Moseley 1969 Neer 1972 Neer 1983 Neviaser Neviaser 1982 Penny and Welsh 1981 Pujadas 1970 Skoff 1995 Smith-Petersen Aufranc 1943 Thorling Bjerneld 1985 Watson-Jones 1960) However the interpretation of these reports is made difficult by the admixture of patients with intact cuffs partial thickness cuff lesions and full thickness cuff tears as well as by the inclusion of a wide range of additional elements to the surgery. Stuart et al (Stuart Azevedo 1990) reported a series which included acromioplasty with or without cuff repair distal clavicle excision and biceps tenodesis; 23% were still painful. Rockwood and Lyons (Rockwood and Lyons 1993) reported on a series of 71 patients who had a modified acromioplasty with or without cuff repair and concluded that cuff repair did not influence the percentage of excellent results. Bosley (Bosley 1991) reported on 35 patients with total acromionectomy including patients with and without long standing massive cuff tears; most failures were attributed to either the underlying pathology or to failure of deltoid reattachment. Bjorkenheim et al (Bjorkenheim Paavolainen 1990) reported a failure rate of over 25% attributing the failures to "associated bony as well as soft-tissue subacromial lesions". Oglvie-Harris et al (Ogilvie-Harris Wiley 1990) evaluated 67 shoulders in 65 patients who had pain and dysfunction for more than two years after an initial acromioplasty for impingement syndrome without a rotator cuff tear. In almost half of the cases there were "diagnostic errors" and even in those where there was a correct diagnosis and no operative errors the failure rate was almost 20%.
Arthroscopic acromioplasty
Ellman (Ellman 1987) in 1987 published the first large series of fifty patients (average age 50 years) with mixed shoulder pathology who under went arthroscopic acromioplasty; ten had full thickness tears. At an average follow-up of seventeen months 88% had good or excellent results. These results persisted at 2.5 year followup of the same treatment group. (Ellman and Kay 1989)
Since then others have reported results of arthroscopic acromioplasty. (Ellman 1987 Esch Ozerkis 1988) Gartsman (Gartsman 1990) Speer et al (Speer Lohnes 1991) Altchek et al (Altchek Warren 1990) and Roye et al (Roye Grana 1995) reported series of arthroscopic acromioplasties on shoulders without cuff tears; each finding 83-94% of the results were satisfactory. Approximately 75% of the patients were able to return to sports activity. Recovery times in these series ranged from 2 to 4 months. Most authors describe the procedure as technically demanding. The control of bleeding and the determination of the amount of bone to resect are two commonly technical difficulties in performing arthroscopic subacromial decompression. Many describe a learning curve associated with this technique and have recommended this procedure be performed on cadaver shoulders before it is used clinically.
In early years after the introduction of the arthroscopic technique of acromioplasty controversy arose as to whether a subacromial decompression performed arthroscopically was technically equivalent to that performed open. Gartsman et al. (Gartsman 1990 Gartsman Blair 1988) in a cadaver study was able to perform arthroscopic bony resection with release of the coracoacromial ligament equivalent to the open technique described by Neer. He suggested criteria for the technical adequacy of the acromioplasty: (1) the entire anterior acromial protuberance is resected (2) the undersurface of the acromion is flattened (3) the deltoid fibers are visible from the acromioclavicular joint to the lateral edge of the acromion (4) the inferior aspect of the acromioclavicular joint is debrided to remove any downward protrusion (5) the coracoacromial ligament is completely released from the anterior portion of the acromion and the acromioclavicular joint (6) a portion of the ligament is resected (7) an adequate subacromial bursectomy is performed to allow complete inspection of the bursal surface of the rotator cuff and (8) finally no subacromial abrasion is observed when the arm is taken through a range of motion at the completion of the procedure.
Most authors state that the indications for arthroscopic acromioplasty should be identical to those for the open procedure described by Neer in 1972. However compared to the rate with which Neer used open acromioplasty in his practice it is apparent that arthroscopic acromioplasty is performed much more commonly with broader indications. Although overall "satisfactory" results were obtained in the majority of reports some authors were uncertain whether relief was obtained from the modifications of the acromial shape or other aspects of the treatment.
To keep things in perspective Brox et al (Brox Staff 1993) compared the effectiveness of arthroscopic acromioplasty an exercise program and a placebo in a randomized clinical trial. The study group consisted of 125 patients aged 18-66 who had had rotator cuff disease for at least three months and whose condition was resistant to treatment. The authors concluded that surgery or a supervised exercise regimen significantly and equally improved rotator cuff disease compared with placebo; however the surgical treatment was substantially more costly.
Comparison of open and arthroscopic acromioplasty
In 1994 Sachs et al (Sachs Stone 1994) reported on a series of 44 patients with stage II impingement prospectively randomized into open (22 patients/average age 49) and arthroscopic treatment groups (19 patients/average age 51). In both groups full recovery took at least 1 year for the majority of patients. In both groups over 90% of patients achieved a satisfactory result (good or excellent). Final analysis showed that the main benefits of arthroscopic acromioplasty were evident in the first 3 months postoperatively with the arthroscopic patients regaining flexion and strength more rapidly than did patients treated with open decompression.
Furthermore the arthroscopic treatment group had shorter hospitalizations used less narcotics and returned more quickly to both work and activities of daily living leading the authors to suggest arthroscopic acromioplasty may have significant economic advantages.
In 1992 Van Holsbeeck et al (van Holsbeeck DeRycke 1992) compared their results of 53 patients treated by arthroscopic acromioplasty and 53 patients treated by an open acromioplasty. Based on the UCLA rating scale good or excellent results were identical for both groups at a 2 year followup. The authors suggested arthroscopic acromioplasty was associated with a shorter recovery time however in the long term there was no difference in strength of forward flexion between the open and arthroscopic groups.
Hawkins at al (Hawkins Saddamis 1992) reported 40% satisfactory results with arthroscopic subacromial decompression while they reported 87% satisfactory results with a concurrent series of open acromioplasty.
Roye et al (Roye Grana 1995) reported a series of 90 arthroscopic acromioplasties and found that the most of the patients who were not throwing athletes obtained satisfactory results and that the presence or absence of a cuff tear did not affect the result.
Lindh et al in 1993 reported on a series of 20 patients who were randomly selected for either open or arthroscopic acromioplasty (10 patients in each group). The average duration of symptoms before surgery was over 5 years. Functional results in both the arthroscopic and open surgery groups were good and similar. Patients in the arthroscopic group were observed to demonstrate earlier restoration of full range of motion and reduction in time away from work.
Proponents of arthroscopic acromioplasty have argued this procedure requires less surgical dissection and produces less scarring and less post operative morbidity. In most instances the procedure can be performed on an outpatient basis. Post operative discomfort is moderate and can usually be controlled by oral analgesics. Additionally cosmesis is good and patient acceptance is high.
A countervailing advantage of open acromioplasty is the advantage of being able to observe directly the subacromial space during motions which preoperatively caused the patient's symptomatic subacromial crepitance and the ability to assure that the crepitance is resolved before the procedure is concluded.
Deltoid retraction can be a significant problem after open procedures which require detachment and subsequent reattachment of the deltoid to the anterior acromion. (Bigliani Cordasco 1988) Arthroscopic acromioplasty has the theoretical advantage of leaving the deltoid origin almost totally undisturbed. However in a recent report Torpey et al (Torpey McFarland 1996) it was pointed out that much of the deltoid arose from the anterior acromion. Their analysis indicated that a 4 mm anterior acromioplasty would detach approximately half of the deltoid fibers whereas a 6 mm anterior acromioplasty would detach approximately 75% of the fibers. They conclude that neither an open nor an arthroscopic acromioplasty can be performed without substantial compromise of the anterior deltoid origin.
Arthroscopy offers the ability to directly inspect the glenohumeral joint as well as subacromial space. During an open acromioplasty the deep surface of the cuff (where most cuff lesions begin) is not visible. By contrast at arthroscopy partial or complete thickness tears of either surface of the rotator cuff as well as other findings can be identified by the experienced observer. However even with arthroscopy the common intratendinous lesions remain inaccessible. Paulos and Franklin (Paulos Harner 1988) in their series of 80 arthroscopic acromioplasties reported a high number of unsuspected diagnoses that were made during arthroscopy. These included twenty-six (26) partial rotator cuff tears twelve (12) labral tears; eight (8) instances of humeral chondrosis; four (4) cases of biceps tendon fraying; and two (2) loose bodies in the glenohumeral joint. They reported that for most of these shoulders these findings would have been missed with the open technique.
Altchek et al (Altchek Warren 1990) in their series of forty-four (44) patients treated by arthroscopic acromioplasty eleven (11) patients had lesions of the glenoid labrum. Preoperatively these patients had no evidence of instability either by history or physical exam in action. Five (5) of these patients had a tear involving the inferior part of the labrum and failed to recover completely after the acromioplasty and were unable to return to full participation in sports. The authors felt that undetected slight instability may have played a role in the production of these patients' symptoms. The authors argued that arthroscopic inspection of the glenohumeral joint makes it possible to detect such problems providing information that is important for prognosis. Others have reported a higher than anticipated percentage of unsuspected associated lesions in those shoulder being treated arthroscopically for impingement symptoms. (Jobe and Kvitne 1989) Burns and Turba (Burns and Turba 1992) reported on their findings in 29 patients treated with arthroscopic acromioplasty which included anterior glenoid labrum tear (15) undersurface rotator cuff tear (8) chondromalacia of the humerus (3) biceps rupture (1) posterior glenoid labrum tear (1) and acromioclavicular arthritis (1).
These results indicate that the preoperative diagnosis of "impingement syndrome" has been associated with a wide range of shoulder pathologies. They leave unanswered the question of the prevalence of these same findings in asymptomatic shoulders and the role played by each of the findings in producing clinical symptoms. Hopefully in the future methodical clinical-pathological correlation will lead to improved accuracy in preoperative diagnosis and greater specificity in treatment.
The primary difficulty in interpreting these studies on open and arthroscopic acromioplasty is that although the outcome of the procedure is characterized in terms such as of "good" or "excellent" the effectiveness of the procedure is often undetermined because the preoperative status or ingo was not characterized in the same way. Ideally a "good" result from surgery would indicate the change in the patient's condition as a result of the procedure rather than the status of the shoulder post operatively.
The definition of the indications for and the effectiveness of acromioplasty must await multipractice studies which define accurately the pretreatment clinical findings and shoulder functional status the nature of and compliance with a non-operative program the nature of the surgery and the change in the shoulder function realized after the procedure using the same parameters of comfort and function before and after surgery. The effectiveness of a treatment is the difference between the outcome and the ingo.
Authors' preferred method for subacromial smoothing
In our experience the results of subacromial smoothing are likely to be best in the following circumstances:
- a well-motivated patient over 40
- absence of posterior capsular stiffness
- presence of symptomatic subacromial crepitus (see figure 20) which the patient agrees is the dominant clinical problem
- absence of tendon signs (see figure 21) and other shoulder pathology and
- symptoms which are not associated with a work-related injury.
Poor prognostic signs include:
- age less than 40
- stiffness
- absence of subacromial crepitus
- presence of tendon signs or evidence of other shoulder pathology
- attribution of problem by the patient to his or her occupation
- concomitant evidence of glenohumeral instability and
- neurogenic cuff muscle weakness.
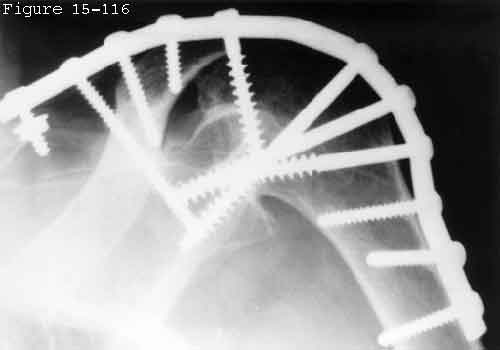
We use an open approach to subacromial smoothing. The patient is positioned with the head up at 30 and the arm draped free. Before making the incision we note the positions and motions in which subacromial crepitus can be palpated through the acromion. The shoulder is approached through an incision in the skin lines over the anterolateral corner of the acromion (see figure 22). The acromion is exposed striving to maintain the continuity of the deltoid fascia the acromial periosteum and the trapezius fascia. The deltoid tendon is split in line with its fibers along the strong tendon of origin that divides the anterior and middle deltoid. This allows two strong "handles" on the deltoid for repair. This split is deepened under direct vision until the bursa is entered. Rotating the humerus provides easy differentiation between the deltoid (which does not move with humeral rotation) and the superficial surface of the cuff (which does).
On entering the subacromial aspect of the humeroscapular motion interface (see figures 23 and 24) the subacromial space is observed while the preoperatively identified crepitus-producing movements are carried out. This step reveals the cause of the crepitance which is usually some combination of roughness on the undersurface of the acromion hypertrophic bursa adhesions between the cuff and acromion roughness of the superior surface of the rotator cuff or a prominent tuberosity. By gently rotating the arm most of the cuff can be brought to the incision as pointed out by Codman. The rotator cuff is thoroughly explored and palpated for evidence of superior surface blisters partial tears thinning or full-thickness defects. Although deep surface cuff fiber failure cannot be seen through this approach it is also true that such fiber disruption cannot be causing the subacromial crepitance. The methylene blue "dye test" of Hiro Fukuda (Fukuda Mikasa 1983) or more recently the "Fukuda-lite" test with saline is used to evaluate shoulders with suspicious cuff integrity. In this test fluid is injected to distend the glenohumeral joint to further explore suspected thinning or small cuff defects.
Hypertrophic bursa is resected. Superior surface cuff defects are smoothed by either resection of their protruding aspects or occasionally by reattaching a superior surface cuff flap. Prominences of the tuberosity are smoothed so that the tuberosity passes easily beneath the coracoacromial arch. The undersurface of the coracoacromial arch is palpated to identify areas of roughness or prominence. These are smoothed with a "pine cone" burr although an osteotome or rongeur may be useful for larger lesions. No attempt is made to resect the coracoacromial ligament unless it can be demonstrated to be the cause of the subacromial roughness.
If a substantial amount of bone needs to be removed a thin-bladed osteotome is used (see figure 25). The osteotomy is oriented in line with the extrapolated undersurface of the posterior acromion (identified by palpation and direct vision). Care is taken that the osteotomy does not continue into the posterior acromion or scapular spine. The undersurface of the acromion is then smoothed using a "pine cone" power bur taking care that no spurs are left laterally in the deltoid origin or medially at the acromioclavicular joint. The shoulder is thoroughly irrigated to remove all bone fragments.
Additional surgery is avoided unless clearly indicated. Inferiorly directed acromioclavicular osteophytes are resected if they scrape on the cuff. The biceps is left undisturbed unless it appears to be seriously inflamed obviously unstable or doomed to imminent rupture in which case we perform a tenodesis to the proximal humerus.
The shoulder is gently manipulated through a complete range of motion to assure the absence of stiffness or additional adhesions. The entire humeroscapular motion interface (see figures 23 and 24) is inspected to assure absence of adhesions and for other pathology. Before the procedure is concluded the upper surface of the cuff and tuberosities and the undersurface of the coracoacromial arch are carefully palpated to assure the absence of residual roughness. The entire range of passive shoulder motion must be free of subacromial crepitance.
On closure a secure deltoid reconstitution is top priority so that early postoperative motion may be instituted. The deltoid is repaired by side-to-side closure of the medial and lateral aspects of the tendon split using No. 2 nonabsorbable suture (see figure 26). The tendon is secured to the acromion using suture to bone as necessary. Suture from the medial hole is passed through the lateral part of the deltoid tendon and suture from the lateral hole is passed through the medial part of the deltoid tendon to effect a crisscross closure. This avoids the "telltale V" defect that reveals a poor deltoid closure. All knots are placed on the superficial aspect to avoid recreating subacromial roughness.
Postoperative program
After any type of subacromial surgery there is a great potential for adhesions between the cuff and the arch. In cases of failed acromioplasty such scarring seems to be a dominant feature and appears to be often related to delay in the institution of motion following the surgery. To avoid such problems we begin motion as soon as possible preferably with continuous passive motion in the recovery room (figure 27). CPM is set to move the arm slowly through an arc of 0 to 90 degrees of elevation and from 50 to 0 degrees of internal rotation. CPM is applied whenever the patient is in bed during their hospitalization but is not continued after discharge. On the day of surgery the patient is instructed in the "140/40 passive program" in which the opposite hand is used to assist the operated shoulder in achieving 140 degrees of elevation (see figure 9) and 40 degrees of external rotation (see figure 11). Emphasis is also placed on posterior capsular stretching including cross body adduction (see figure 14) reaching up the back (see figure 13) and internal rotation of the abducted arm.
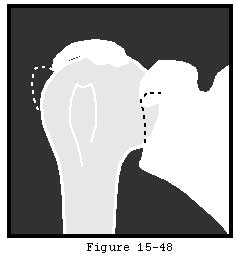
The early implementation of passive motion is facilitated if the procedure is performed under brachial plexus block (Tetzlaff Yoon 1994) which lasts from 12 to 18 hours. The post operative exercises are already familiar to the patient having been performed as part of the preoperative trial of the Jackins program. The patient is allowed active use of the shoulder within the realm of comfort unless there is concern for the strength of the deltoid reattachment. Internal (see figure 15) and external rotation (see figure 16) strengthening exercises are also begun immediately. Deltoid strengthening is initiated at 6 weeks after the repair is secure (see figure 17). As soon as they can be performed comfortably exercises to strengthen the scapular motors are added (see figures 18 and 18). Athletics are not allowed for three months after surgery and until normal motion and strength are regained.
Failed acromioplasty
In this condition the patient is dissatisfied with the result from a previous arthroscopic or open acromioplasty and presents for consideration of additional surgery.
Failure to achieve relief of symptoms
Such results occur in every series of acromioplasty even if the technique of the procedure seems appropriate. The incidence of these failures ranges from 3 to 11 per cent. (Neer 1972 Post and Cohen 1985 Raggio Warren 1985 Thorling Bjerneld 1985) In Post and Cohen's series 11 per cent continued to have significant pain after surgery. (Post and Cohen 1985 Post and Cohen 1986) Fifty-six per cent of those with weakness before surgery still had weakness postoperatively; 29 per cent of those with preoperative limitations of motion still had limitation of motion after surgery. The rate of return to high-level athletics or challenging occupations is lower. Tibone and colleagues (Tibone Jobe 1985) found that of 35 athletes having impingement syndrome treated by anterior acromioplasty 20 per cent still had moderate to severe pain and 9 per cent had pain at rest and with activities of daily living. Only 43 per cent returned to their preinjury level of competitive athletics and only 4 of 18 returned to competitive throwing. Hawkins and coworkers (Hawkins Chris 1987) have shown that it is difficult for patients injured on the job to return to their original occupations following acromioplasty.
Why is this? Failure to achieve complete relief of symptoms through acromioplasty may indicate:
- pathology other than subacromial roughness
- failure to achieve subacromial smoothness
- failure of deltoid reattachment
- excessive acromial resection
- postoperative complications such as dense scarring between the cuff and the acromion or
- failure of rehabilitation.
Many of these problems can leave the patient more symptomatic than before the surgery.
Acromioclavicular joint problems were thought to be responsible for five failures in Post's series a "frequent cause of failure of surgical treatment" in the series of Penny and Welsh (Penny and Welsh 1981) and the cause of the only unsatisfactory result in Neer's series. In their series of patients having persisting problems after acromioplasty Hawkins and colleagues (Hawkins Chris 1987) reported that forty-five per cent of the patients had a diagnosis other than continuing impingement including acromioclavicular joint problems cervical spondylosis reflex sympathetic dystrophy rotator cuff tear thoracic outlet syndrome glenohumeral osteoarthritis and glenohumeral instability. Thirty-three per cent were thought to have continuing subacromial abrasion. The striking finding in this series was the relative lack of improvement in patients on workmen's compensation after revision acromioplasty. Even in these authors' series of primary acromioplasties twenty-two per cent of the workmen's compensation cases had an unsatisfactory result compared with eight per cent failure rate with non--workmen's compensation cases. (Hawkins and Brock 1979) Post and Cohen (Post and Cohen 1986) also observed that worse results were obtained from surgery performed for work-related impingement syndrome. This inability to return to work may be due to partial-thickness cuff tears residual tendon scarring and residual weakness. Post and Cohen emphasized the need for recovery of muscle strength before the laborer is returned to work; otherwise recurrence can be anticipated. The difficulty of returning workers to their jobs after acromioplasty is reminiscent of the problems described by Tibone and coworkers (Tibone Jobe 1985) in returning athletes to a competitive level of function.
Bosley (Bosley 1991) reported that most failures were attributed to either the underlying pathology or to failure of deltoid reattachment. Bjorkenheim et al (Bjorkenheim Paavolainen 1990) reported a failure rate of over twenty-five per cent attributing the failures to "associated bony as well as soft-tissue subacromial lesions". Oglvie-Harris et al ( Ogilvie-Harris Wiley 1990) evaluated 67 shoulders in 65 patients who had pain and dysfunction for more than two years after an initial acromioplasty for impingement syndrome without a rotator cuff tear. In almost half of the cases there were "diagnostic errors" and even in those where there was a correct diagnosis and no operative errors the failure rate was almost twenty per cent.
Radical acromionectomy may worsen a patient's comfort and function. This procedure removes the origin of the deltoid muscle and facilitates scar formation between the deltoid muscle and the rotator cuff. Neer and Marberry have pointed out that a radical acromionectomy may seriously compromise shoulder function without achieving subacromial smoothness. (Neer and Marberry 1981) In their series of thirty patients all had marked shoulder weakness and almost all had persistent pain. In the twenty shoulders reoperated upon all had a retracted and scarred middle deltoid that was adherent to the cuff and humerus. Fifteen of the patients had residual cuff tears. Attempts to reconstruct these severely damaged shoulders were disappointing. The effects of loss of the deltoid attachment and the permanent contracture could not be reversed. In addition these authors observed a high incidence of wound problems and infections following the radical acromionectomy which further complicated their attempts at revision.
To help understand some of the other causes of unsuccessful acromioplasty Flugstad and coworkers (Flugstad Matsen III 1986) reviewed nineteen patients referred to the University of Washington Shoulder and Elbow Service because of persistent pain and stiffness after open acromioplasty performed elsewhere. The average age was 42; 16 were male. Eleven patients had a traumatic onset of their shoulder problem; eight of these were work related. The average time of postoperative immobilization was four weeks. At the time of presentation the patients complained of pain and stiffness. Physical examination revealed an average of 126 degrees of forward flexion and 36 degrees of external rotation and internal rotation so that the thumb could touch T12. In thirteen of these patients revision surgery was performed after an exercise program failed to improve their symptoms. The average interval between the initial surgery and revision surgery was fifteen months. At the revision surgery ten patients had roughness of the undersurface of the acromion. Five patients had distinct spurs protruding from the lateral or medial acromion; eight patients had large amounts of subacromial scarring in which heavy bands of cicatrix connected the undersurface of the acromion to the rotator cuff. Three patients had acromioclavicular joint spurs one had a large ununited acromial fragment and another had an os acromial. Although no patient had a full-thickness cuff tear the incidence of partial-thickness deep surface or midsubstance cuff tears is unknown. The revision surgical procedure included excision of scar tissue revision of the acromioplasty to assure adequate resection of the anterior and inferior acromion resection of acromioclavicular spurs inspection of the rotator cuff and careful deltoid repair. Immediately after surgery gentle range-of-motion exercises were initiated to minimize restriction from postoperative scar. Follow-up at an average of ten months postoperatively revealed substantial although incomplete improvement in comfort range of motion and ability to work.
This report emphasizes the importance of accurate diagnosis and effective subacromial smoothing. However the key lesson was the importance of rapid restoration of full joint motion before restricting adhesions have the opportunity to form: the average patient in this series had a one-month delay between surgery and the implementation of motion.
Authors' preferred method for the management of failed acromioplasty
Patients who have had previous acromioplasty with unsatisfactory results need to be carefully reevaluated to determine presence of stiffness weakness instability or persisting roughness. The social and vocational context of the shoulder problem must be reevaluated as well.
The Jackins non-operative program is instituted even if the patient has already "had therapy"; since surgery has failed once already there is plenty of time for conservatism and a period of observation.
Patients with positive tendon signs (see figure 29) may be considered for cuff imaging studies if these signs are refractory to rehabilitation. Vocational rehabilitation may be essential; if one procedure has not gotten the patient back to their job the odds would seem not much better the second go-round.
Reoperation is considered in well-motivated patients with evidence of residual subacromial roughness or stiffness that is attributable to postoperative scarring in the humeroscapular motion interface (see figures 30 and 31). In contrast to primary acromioplasty we are willing to reoperate on patients with refractory shoulder stiffness because this stiffness may be due to dense scarring between the cuff and the acromion which cannot be managed nonoperatively. Our revision procedure is identical with the primary subacromial smoothing described earlier.
Partial thickness cuff lesions
In this condition partial thickness disruption of the cuff is manifest by pain or weakness on resisted isometric contraction of the involved cuff muscles.
Signs and symptoms
The shoulder commonly demonstrates associated posterior capsular tightness. Imaging studies may indicate cuff tendon thinning or partial thickness defects but the lesion does not extend through the full thickness of the tendon.
Intrasubstance and articular surface
Judging from the cadaver studies reviewed earlier in this chapter intrasubstance and articular surface partial thickness cuff tears represent the commonest forms of cuff involvement. These lesions usually involve the supraspinatus tendon near its anterior insertion but may also involve the infraspinatus and subscapularis. Clinical observation of patients with documented partial thickness cuff lesions suggests that they produce symptoms analogous to other partial thickness tendon lesions such as a partial Achilles tear a partial tear of the patellar tendon or a partial tear of the tendon of origin of the extensor carpi radialis brevis ("tennis elbow"). These partial tendon lesion symptoms include stiffness of the joint on passive motion in a direction that stretches the tendon and tendon signs i.e. pain or weakness on isometric contraction of the tendon's muscle (see figure 32). These partial tendon lesions are often much more painful than full thickness tears. This is because in contrast to full thickness tears partial thickness defects of the cuff give rise to stiffness and unphysiologic tension on the remaining fibers. In its less common form involving the bursal aspect of the cuff tendon partial thickness cuff lesions may be associated with subacromial abrasion yielding subacromial crepitance on passive joint motion. There is not a lot of published information regarding the results of operative treatment for partial thickness cuff lesions. Fukuda and colleagues (Fukuda Mikasa 1983 Fukuda Mikasa 1987) described the management of six patients with partial-thickness bursal-side tears by acromioplasty and/or wedge resection with tendon repair to bone. They used an intraoperative "color test" in which dye was injected into the shoulder joint to indicate the extent of joint side tears. The results were satisfactory in 90 per cent of cases. Itoi and Tabata (Itoi and Tabata 1992b) reported their results in managing 38 shoulders with partial thickness cuff lesions. The average follow-up period of 4.9 years and the average age at operation was 52.2 years. Three types of lesions were identified: superficial (12 shoulders) intratendinous (three) and deep surface tears (23). The authors performed full-thickness resection of the cuff including the lesion and repaired the defect with side-to-side suture (13 shoulders) side-to-bone suture (eight) fascial patch grafting (16) or side-to-bone suture with fascial patch grafting (one). The overall results were satisfactory in 31 shoulders (82%). The results were not affected by the tear types operative methods or follow-up period.
Arthroscopic treatment
Andrews et al (Andrews Broussard 1985) presented thirty-six patients with partial thickness tears of the supraspinatus portion of the cuff treated with arthroscopic debridement of the rotator cuff defect. No acromioplasty was performed. The average age was 22.5 and 64% of the patients were baseball pitchers. Of the 34 patients available for follow-up 85% had an excellent (26 patients) or good (3 patients) result and were able to return to sports. The authors suggested that the debridement may initiate a healing response. Arthroscopy revealed a tear of some part of the glenoid labrum in all patients. Six had partial tears of the long head of the biceps tendon. These observations point to the difficult of deciding which surgical findings are responsible for the patient's symptoms. Ogilvie-Harris and Wiley (Ogilvie-Harris and Wiley 1986) reported on arthroscopic treatment of 57 incomplete tears of the rotator cuff with symptoms of impingement. These tears were debrided and no acromioplasty was performed. Half of the patients improved. Wiley (Wiley 1985) reported on thirty-three patients treated arthroscopically for partial tears of the rotator cuff. Only three patients achieved a satisfactory result. Ellman reported good results from arthroscopic acromioplasty performed in conjunction with arthroscopic debridement of partial thickness tears of the rotator cuff. (Ellman and Kay 1991) Esch et al (Esch Ozerkis 1988) in 1988 reported on thirty-four patients with stage II rotator cuff disease and partial thickness rotator cuff tears treated with arthroscopic acromioplasty and tear debridement. Twenty-eight patients were satisfied with their results; 16 patients were rated excellent 10 were good 6 were fair and 2 were rated as poor. Gartsman (Gartsman 1990) presented forty patients with partial thickness rotator cuff tears in a group of 125 patients treated with arthroscopic acromioplasty. Of these partial thickness tears thirty-two involved the articular surface of the supraspinatus tendon and four tears involved the bursal side. Four infraspinatus tears were identified three of which involved the articular surface. Notably in these forty patients there were twenty-seven cases of labral fraying with six instances of biceps/labral complex detachment again indicating the difficulty of relating symptoms to surgical findings. Of the forty patients thirty-three (83% satisfactory results) had major improvement in their ratings for pain activities of daily living work and sports at an average of 28.9 months post-arthroscopic debridement. Two patients who had an unsatisfactory result had a second operation: one open acromioplasty and the other repair of the rotator cuff with satisfactory results. Of the thirty patients in this group engaged in sports preoperatively ten patients returned to those sports at the same level of performance as before the symptoms had started. Altchek et al (Altchek Warren 1990) reported four of six good or excellent results in patients with partial thickness rotator cuff tears treated with arthroscopic acromioplasty and debridement of the rotator cuff defect. Roye et al (Roye Grana 1995) presented thirty-eight patients with partial thickness rotator cuff tears (thirty-two involving the supraspinatus) treated with arthroscopic acromioplasty. A satisfactory result was achieved in 95%. As part of a larger series Ryu (Ryu 1992) reported on thirty-five patients with partial thickness rotator cuff tears treated with arthroscopic acromioplasty. Thirty of thirty-five patients (86%) were rated with excellent or good results (5 fair no poor) at a minimum follow-up of 12 months. Of the group with partial tears four were found to involve only the articular surface. Three of these four were considered failures In 1994 Olsewki and Depew (Olsewski and Depew 1994) reported on their experience with 61 consecutive patients treated with arthroscopic acromioplasty and debridement of the rotator cuff defect (17 of 21 patients (81%) with a partial thickness rotator tear rated a satisfactory result (UCLA rating scale). This was identical to the result achieved in 27 patients treated with arthroscopic acromioplasty for rotator cuff "tendonitis" with an intact rotator cuff. As was the case with the series of Roye et al (Roye Grana 1995) the extent of the tear did not statistically affect the result. From this group of reports it is difficult to define (1) the indications for surgery (2) which aspects of the patients' pathologies were responsible for their symptoms (3) why from 15-50% of patients failed to achieve a satisfactory result and (4) which aspect of the surgery (acromioplasty or debridement) was responsible for improvement after surgery. It seems likely that those patients benefiting from this procedure were able to heal their tendon debridement in a way that stabilized the insertional mechanism distributing the loads from muscle to bone in a way that prevented disproportionately large loads from being concentrated on the neighboring intact tendon fibers.
Authors' preferred method of treating partial thickness cuff lesions
Nonoperative treatment
The nonoperative management of partial thickness cuff tears is similar to that for subacromial abrasion described earlier in this chapter.Just as with partial lesions of the Achilles patellar or extensor radialis brevis tendons the program must emphasize stretching against all directions of tightness including internal rotation (see figure 33) cross-body adduction (see figure 34) elevation (see figures 35 and 36) and occasionally external rotation (see figure 37). As in a tennis elbow rehabilitation program when a comfortable normal range of passive motion is reestablished gentle progressive muscle strengthening is instituted (see figures 38 and 39) An emphasis is always placed on gentle and comfortable progress of this rehabilitation program. The goal of this program is to assure that the scar collagen which forms in the defect will become as supple as normal tendon; otherwise scar contracture will tend to concentrate the loads of the cuff on the lesion leading to recurrence and propagation of injury.
Operative treatment - Open surgery
Just as is the case for partial Achilles patellar and extensor carpi radialis brevis tendon lesions there is no surgical treatment which reliably restores the tendon to its normal condition. Preoperatively it is important to determine whether the patient's primary problem is due to stiffness or to difficulties upon active muscle contraction so that the procedure can be biased accordingly. On the one hand sectioning of the fibers which remain intact (as in a tennis elbow release) may worsen the problem of weakness; although this may be the basis of the arthroscopic "debridement" advocated by some surgeons for this lesion. On the other hand excision of the defect and repair would worsen the problem of stiffness. (Zuckerman Leblanc 1991) Furthermore such surgical tightening of involved part of the cuff would cause the area of damage and repair to bear the majority of the load when the cuff muscles contract (reminiscent of the "quadregia" phenomenon in hand surgery). Thus excision and repair of partial thickness cuff lesions should include efforts to assure that the tendon load is distributed evenly at the insertion by carrying out a repair that is isometric allowing uniform load distribution and by carrying out a release of the capsule tightened in the repair. (Harryman Matsen 1996) The surgical exposure to the partial thickness cuff lesion is identical to that described for the management of subacromial roughness (see figure 40). If symptoms are related to subacromial abrasion (i.e. symptomatic subacromial crepitance) subacromial smoothing is performed as described previously in this chapter. The decision to convert a partial thickness cuff defect to a full thickness defect and then to repair it (see figure 41) is based on the patients preoperative evaluation and surgical findings. The thickness of the cuff can be determined at surgery by inspection palpation and the Fukuda test described above. A depth gauge or calibrated nerve hook inserted in the area of the lesion may help determine the percentage of the tendon that remains intact. If the decision is made to perform an open repair a tenotomy is performed in the most suspicious area along the line of the tendon fibers to explore the full thickness of the tissue. If as is usually the case the defect is within the substance of the tendon or on its deep surface near the anterior insertion of the supraspinatus a longitudinal tenotomy and capsulotomy are performed along the anterior aspect of the supraspinatus near the rotator interval. This cut is then extended at right angles posteriorly through the partially detached cuff at its insertion to the greater tuberosity turning back the flap of cuff until normal tendon of full thickness is encountered. Next an attempt is made to retrieve and consolidate any split laminations of cuff which may have retracted medially (see figure 41). These are usually on the deep articular surface where the cuff lesion begins and may have retracted up to 1 cm. Release of the coracohumeral ligament and the rotator interval capsule from the base of the coracoid (see figures 42 and 43) as well as release of the capsule from the glenoid lip (see figure 44) will minimize tension on the repair. Then the full thickness defect is repaired (see figures 45 and 46) with care to render the cuff insertion isometric with respect to all it fibers and smooth on its superior surface. Finally with the anterior undersurface of the acromion in full view the shoulder is put through a full range of motion to verify the elimination of any subacromial abrasion (see figure 47) and to assure that the repair has not restricted shoulder motion. Postoperative management is the same as for the repair of full thickness defects with a particular emphasis on continuous passive motion (see figure 48) and on the early restitution of a full range of motion to prevent stiffness and adhesions (see figures 34 35 36 37 49 and 50).
Full thickness cuff tears
Characteristically full thickness cuff tears present as pain or weakness on resisted isometric contraction of one or more of the cuff muscles.
Diagnosis
A full thickness defect of one or more of the cuff tendons can be demonstrated on ultrasonography arthrography MRI arthroscopy or open surgery.
While the diagnosis is not difficult a number of key factors must be considered in selecting the appropriate treatment for cuff defects.Some defects cannot be repaired because as McLauglin pointed out they offer only "rotten cloth to sew" (McLaughlin 1944 McLaughlin 1962 McLaughlin 1963 McLaughlin and Asherman 1951) The recognition that full thickness cuff tears may exist without clinical symptoms (Harryman Mack 1991 Matsen Lippitt 1994 Milgrom Schaffler 1995 Pettersson 1942 Sher Uribe 1995) cautions that cuff defects need not be repaired just because they are there.
Nonoperative treatment
Substantial data are available on the results of nonoperative treatment for full thickness cuff defects. The programs generally include some combination of "compound tincture of time" along with physical therapy administration of nonsteroidal anti-inflammatory medications rest avoidance of precipitating activities and steroid injections.
Improvement with nonoperative management was noted to be 33 per cent in Wolfgang's series (Wolfgang 1978) 44 percent in Takagishi's series (Takagishi 1978) 59 percent in Samilson and Binder's series (Samilson and Binder 1975) and 90 percent in Brown's series. (Brown 1949)
Steroid injections do not seem to be a major enhancement to the nonoperative management program. Although Weiss (Weiss 1981) presented some evidence that patients with arthrographically proven cuff tears are symptomatically improved by intra-articular injections there is little evidence for a protracted benefit from this method. Other observers found that steroid injections offered no benefit to patients with cuff tears. Coomes and Darlington (Coomes and Darlington 1976 Darlington and Coomes 1977) Lee and colleagues (Lee Lee 1974) and Connolly (Connolly 1972) compared steroid and local anesthetic injections in patients with tendinitis and tendon tears. They found a small subjective benefit in relief of pain but no effect on function in the steroid-treated group.
There has been a recent resurgence of reports confirming the value of nonoperative management for chronic cuff tears. Bartolozzi et al (Bartolozzi Andreychik 1994) studied the factors predictive of outcome in 136 patients with cuff disease who were treated nonoperatively. Mean followup was 20 months (range 6-41 months). The authors found 66-75% good or excellent results with indication that the clinical result improved significantly as followup duration increased. Prognostic factors that were associated with an unfavorable clinical outcome included a rotator cuff tear over one square centimeter a history of pretreatment clinical symptoms for over one year duration and significant functional impairment at initial presentation.
Hawkins and Dulap (Hawkins and Dunlop 1995)found that over half of patients with full thickness cuff tears treated with a supervised nonoperative program of rotator strengthening exercises obtained satisfactory results at an average of four years followup. Bokor et al (Bokor Hawkins 1993) managed 53 patients (average age 62 years) with full thickness cuff tears documented arthroscopically using a program of non-steroidal medications stretching strengthening and occasional steroid injections. At an average of 7.6 years later thirty-nine of the 53 patients (74%) had only slight or no shoulder discomfort. Of the 28 shoulders presenting within three months of injury 24 (86%) were rated as satisfactory at the time of latest evaluation. Of the 16 patients who initially had had shoulder pain for over 6 months only nine (56%) were rated as satisfactory. Most patients showed improvement with regard to their ability to perform activities of daily living. Average active total elevation was 149 degrees compared with 121 degrees at initial presentation. Thirty-two of the 34 patients examined (94%) had evidence of weakness on muscle testing and 19 (56%) had demonstrable muscle atrophy.
Itoi and Tabata (Itoi and Tabata 1992a) followed 62 shoulders with complete rotator cuff tears which were treated conservatively from 1980 until 1989. The follow-up period averaged 3.4 years. Fifty-one shoulders (82%) rated satisfactory. The overall scores of pain motion and function improved significantly. The authors concluded that conservative treatment affords satisfactory results when it is given to the patients with well-preserved motion and strength although in some cases function may deteriorate with time.
In our own practice we have followup data on 56 patients (23 female 33 male) with full thickness cuff tears managed nonoperatively. The average age was 61 ± 10 years (range 45-84) and the mean followup time was 25 months. The initial and final responses to the questions of the Simple Shoulder Test are shown in table 1 below.
Table 1
| Effectiveness of Non Operative Management of Full Thickness | ||
| Cuff Tears (56 Patients Average Follow-up 25 Months) | ||
| Function | % Able Initially | % Able At Follow-up |
| Sleep on side | 27 | 48 |
| Arm comfortable at side | 57 | 80 |
| Wash back of opp. shoulder | 36 | 41 |
| Place hand behind head | 52 | 65 |
| Tuck in shirt | 57 | 70 |
Taken together these results clearly offer encouragement for a trial of nonoperative management for chronic full thickness cuff tears particularly in cases where the prospect of achieving a durable cuff repair appears doubtful.
Operative treatment
Cuff repair
Patient Selection
Substantial information bearing on the potential reparability of a rotator cuff defect can be obtained from the history along with the physical examination and plain radiographs (see table 2).
Table 2
| Prognostic Factors Related to the Durability of Rotator Cuff Repair | |
| ENCOURAGING | DISCOURAGING |
| History | |
| Age less than 55 | Age over 65 |
| Acute traumatic onset | Insidious atraumatic onset |
| No relation to work | Attribution of tear to work |
| Short duration of weakness | Weakness over 6 months |
| No history of smoking | Many smoking pack-years |
| No steroid injections | Repeated steroid injections |
| No major medications | Systemic steroids or antimetabolites |
| No concurrent disease | Inflammatory joint disease other chronic illnesses |
| No infections | History of previous shoulder infection |
| No previous shoulder surgery | Previous cuff repair attempts |
| Benign surgical history | History of failed soft tissue repairs (e.g. dehiscence infections complicating herniorrhaphy) |
| Physical examination | |
| Good nutrition | Poor nutrition |
| Mild-moderate weakness | Severe weakness |
| No spinatus atrophy | Severe spinatus atrophy |
| Stable shoulder | Anterior superior instability |
| Intact acromion | Previous acromial resection |
| No stiffness | Stiffness |
| X-rays | |
| Normal radiographs | Upwards displacement of head against coracoacromial arch Cuff tear arthropathy |
Acute tears in younger healthy individuals without prior shoulder disease are more likely to be repairable. Long-standing tears associated with major weakness in older patients carry a poorer prognosis. The prognosis for a durable repair is even worse if the history reveals the administration of local or systemic steroids smoking or difficulties in healing previous injuries or surgeries.
These guidelines are derived from our experience but also are supported by the literature. Postacchini et al (Postacchini Perugia 1992) found in a study of 73 cuff repairs that while seventy-three percent of the cases had satisfactory results rotator cuff repair is almost always successful in patients with more than 60 degrees of active arm flexion and either small or medium-size tears. Less than two-thirds of the patients with major tears and less than 60 degrees of motion achieved satisfactory results particularly if there was cuff muscle atrophy.
Watson (Watson 1985) reviewed the surgical findings in 89 patients with major ruptures of the cuff. He found that all seven patients who had had no local steroid injections had strong residual cuff tissue. Thirteen of 62 patients having one to four steroid injections had soft cuff tissue that held suture poorly; 17 of the 20 patients having more than four steroid injections had very weak cuff tissue; these shoulders with weak cuff tissue had poorer results after surgical repair.
Misamore et al (Misamore Ziegler 1995) evaluated 107 consecutive cuff repairs including 24 patients on Workers' Compensation and 79 who were not. Although other factors such as the age and sex of the patients the size of the tear of the rotator cuff and the preoperative strength pain and active range of motion of the shoulder were comparable only 54 per cent of the shoulders covered by Workers' Compensation were rated good or excellent compared with 92 per cent who were not. Forty-two per cent of the patients on Workers' Compensation returned to full activity compared with 94 per cent who were not.
Samilson and Binder listed the following most reasonable indications for operative repair of non-acute cuff tears: (Samilson and Binder 1975)
- a patient "physiologically" younger than 60 years
- clinically or arthrographically demonstrable full-thickness cuff tear
- failure of patient to improve under nonoperative management for a period not less than six weeks
- patient's need to use the involved shoulder in overhead elevation in his or her vocation or avocation
- full passive range of shoulder motion
- patient's willingness to exchange decreased pain and increased external rotator
- strength for some loss of active abduction and
- ability and willingness of the patient to cooperate.
Grana et al (Grana Teague 1994) reviewed their experience with 54 patients having open repair of chronic cuff tears. They concluded that pre repair arthroscopic evaluation did not affect the functional outcome but did increase the cost by about $2000 per patient.
Laboratory studies on repair techniques
Gerber et al (Gerber Schneeberger 1994) studied the mechanical properties of several techniques of tendon-to-bone suture employed in rotator cuff repair in cadavers. Two simple stitches failed at 184 N; four simple stitches failed at 208 N. Two Mason-Allen stitches failed at 359 N. These results indicate that in addition to the quality of the bone and the quality of the cuff tissue the number of sutures and the suture technique affect the load to failure.
Technique of cuff repair
A most important recent study bearing on the technique of cuff repair was published by Zuckerman et al. (Zuckerman Leblanc 1991) These authors used a cadaver model to determine the effect of arm position and capsular release on the tension in the repaired tendon as reflected by strain gauges on the greater tuberosity. They found that with repair of supraspinatus-only defects tension in the repair increased significantly as the arm was lowered from 30 to 15 degrees of abduction. Release of the capsule from the glenoid rim (see figures 51 and 52) significantly reduced the tension at 15 and 0 degrees of abduction. For tears involving the supraspinatus and infraspinatus abduction of at least 30 degrees was required to reduce tension in the repair. Release of the capsule from the glenoid (figure 52) resulted in a 30% reduction in repair tension when the arm was adducted.
Warner et al (Warner Krushell 1992) studied the relationships of the suprascapular nerve to the cuff muscles in thirty-one cadaveric shoulders. The suprascapular nerve ran an oblique course across the supraspinatus fossa was relatively fixed on the floor of the fossa and was tethered underneath the transverse scapular ligament. In eighty-four percent of the shoulders there were no more than two motor branches to the supraspinatus muscle and the first was always the larger of the two. In eighty-four per cent the first motor branch originated underneath the transverse scapular ligament or very near it. In one shoulder (3 percent) the first motor branch passed over the ligament. The average distance from the origin of the long tendon of the biceps to the motor branches of the supraspinatus was three centimeters. In forty-eight percent the infraspinatus muscle had three or four motor branches of the same size. The average distance from the posterior rim of the glenoid to the motor branches of the infraspinatus muscle was two centimeters. The motor branches to the supraspinatus muscle were fewer usually smaller and significantly shorter than those to the infraspinatus muscle. The standard anterosuperior approach allowed only one centimeter of lateral advancement of either tendon and limited the ability of the surgeon to dissect safely beyond the neurovascular pedicle. The advancement technique of Debeyre et al. or a modification of that technique permitted lateral advancement of each muscle of as much as three centimeters and was limited by tension in the motor branches of the suprascapular nerve. In some situations the safe limit of advancement may be even less. The authors concluded that lateral advancement of the rotator cuff is limited anatomically and may place the neurovascular structures at risk.
Surgical approaches
The surgical approaches to the complete cuff tear vary substantially. These include a saber cut (Codman 1911) an anterior approach through the acromioclavicular joint (Bateman 1963) a posterior approach (Debeyre Patte 1965) and an "extensile" approach. (Ha'eri and Wiley 1980) Many authors prefer the anterior acromioplasty approach taking care to preserve the deltoid attachment and acromial lever arm. (Cofield 1981 Cofield 1985 Neer 1972 Neer and Marberry 1981) This technique provides excellent exposure of the common sites of lesions--the anterior cuff biceps groove undersurface of the acromion and acromioclavicular joint.
Packer and coworkers (Packer Calvert 1983) reporting on 63 cuff repairs followed for an average of 32.7 months found that those performed with acromioplasty yielded more pain relief than cuff repair without acromioplasty. If greater access to the supraspinatus is needed the acromioclavicular joint can be excised. (Neer 1983) Debeyre and associates (Debeyre Patte 1965) described a posterior approach with acromial osteotomy. Ha'eri and Wiley described an approach that is extensile through the acromioclavicular joint to the supraspinous fossa. (Ha'eri and Wiley 1980)
Repair methods
Operative techniques for repairing full-thickness cuff defects include tendon-to-tendon repair and tendon advancement to bone. McLaughlin (McLaughlin 1944 McLaughlin 1962 McLaughlin 1963 McLaughlin 1994 McLaughlin and Asherman 1951)described his approaches to transverse ruptures (reinsertion into bone) longitudinal rents (side-to-side repair) and tears with retraction (side-to-side repair followed by reinsertion of the retracted portion of cuff into the head wherever it will reach with ease with the arm at the side). Although many of his principles are still applied today most authors would not concur with his use of the transacromial approach or his belief that "distinct benefits are gained by excising and discarding the outer fragment of the divided acromion." (McLaughlin 1944 McLaughlin 1963) Hawkins and colleagues used side-to-side repair for small tears and tendon-to-bone repair for larger defects. (Hawkins Misamore 1985) Cofield has emphasized the identification of the tear pattern and the use of direct repair and flaps as indicated by the tear pattern. (Cofield 1982 Cofield 1985) Nobuhara et al (Nobuhara Hata 1994) reviewed at an average of seven years one hundred eighty-seven patients (189 shoulders) treated surgically for massive rotator cuff tears using either a tendon-to-tendon repair or the McLaughlin procedure. Ninety-five per cent of the patients were 45 years or older. Excellent or good functional results were attained in 93% of patients. Thirty-three percent of those who underwent tendon to tendon repair complained of pain after overuse compared with only 18% who had the McLaughlin Procedure.
A number of authors have described extensive tendon mobilization or advancement of major tendon flaps to repair large defects. Cofield recommended the transposition of the subscapularis for repair of large cuff defects. (Cofield 1982) In this technique the subscapularis and the anterosuperior capsule are freed from the anteroinferior capsule leaving the middle and inferior glenohumeral ligaments intact. The tendon is then transferred superiorly to the anterior aspect of the greater tuberosity. Most patients required postoperative protection in an abduction splint or cast for four to five weeks. These patients who had severe symptoms of pain and limitation of function preoperatively had less pain and slight improvement in active motion; 12 of 26 patients gained more than 30 degrees of active abduction and 4 lost this amount of motion. Two patients disrupted their repair during the acute postoperative period. Of the twenty-six twenty-five were satisfied with the procedure.
Karas and Giachello (Karas and Giachello 1996) recently reported their results with twenty patients treated with acromioplasty and subscapularis transfer for massive (>5 cm) tears of the cuff in which direct tendon to bone reconstruction could not be achieved. At a mean of 30 months after surgery seventeen patients were satisfied. Nine had weakness and discomfort with overhead activities and two had lost active elevation despite relief of pain. The authors found this procedure useful when "traditional" methods of repair were insufficient but cautioned against its use when patients had full functional elevation preoperatively.
In less than five per cent of his cuff repairs Neer (Neer 1983) shifted the infraspinatus and upper half of the subscapularis superiorly to close a defect in the supraspinatus leaving the lower half of the subscapularis the teres minor and the intervening capsule intact. He described the use of a second incision posteriorly for better mobilization of the infraspinatus toward the top of the greater tuberosity. Neviaser and Neviaser (Neviaser and Neviaser 1982) described the transposition of both the subscapularis and the teres minor to close the defect. Debeyre and colleagues and others described the use of a supraspinatus muscle slide to help close major cuff defects. (Debeyre Patte 1965 Ha'eri and Wiley 1980 Ha'eri and Wiley 1981) Ha'eri and Wiley (Ha'eri and Wiley 1981) used the supraspinatus advancement technique of Debeyre; most of their 18 patients achieved satisfactory results.
Latissimus transfers as described for Erb's palsy (Phipps and Hoffer 1995) have been used to manage large cuff defects. Gerber (Gerber 1992) reported on sixteen irreparable massive rotator cuff tears treated with latissimus dorsi transfer and reviewed after an average of 33 months. Pain relief was satisfactory in 94% of the shoulders at rest and in 81% on exertion. Flexion was 83 degrees preoperatively and 135 degrees postoperatively. If the subscapularis was torn and could not be adequately repaired latissimus dorsi transfer was of no value. In cases with good subscapularis function but irreparable defects in the external rotator tendons restoration of approximately 80% of normal shoulder function was obtained.
A flap of deltoid has been used to cover cuff defects. Thur and Julke (Thur and Julke 1995) analyzed the results of shoulder reconstruction using an anterolateral deltoid muscle flap plasty in 100 patients with rotator cuff lesions which were at least 5 x 5 cm in size. Ninety per cent of patients were satisfied. Shoulder function improved significantly and 72% recovered their strength completely. Most of the patients were able to work after six months. The overall result was good to very good in 83%.
Dierickx and Vanhoof (Dierickx and Vanhoof 1994) reviewed twenty patients with a painful massive irreparable rotator cuff tear treated with an open partial acromionectomy and an anterior deltoid muscle inlay flap. After follow-up averaging 12 months 17 out of 20 patients were satisfied and the UCLA score improved from an average of 9.35 to an average of 25.7 Active forward flexion improved in 17 and strength of forward flexion improved in 15 patients.
As an alternative approach to surgery for massive tears Burkhart et al (Burkhart Nottage 1994) repaired the margins of the tear to restore force transmission believing that complete coverage of the defect was not essential. In fourteen patients this procedure led to improvement in active elevation from 59.6 degrees to 150.4 degrees. Strength improved an average of 2.3 grades on a 0-to-5-point scale. The average score on the UCLA Shoulder Rating Scale improved from a preoperative value of 9.8 to a postoperative value of 27.6. All but one patient was very satisfied
Some authors have used biological and prosthetic grafts to repair large cuff defects. Neviaser (Neviaser 1971) Bush (Bush 1975) and McLaughlin and Asherman (McLaughlin and Asherman 1951) employed grafts from the long head tendon of the biceps to patch cuff defects. Ting and coworkers (Ting Jobe 1987) found that the electromyographic activity and size of the long head tendon of the biceps is significantly greater in patients with cuff tears compared with the uninjured shoulder. Their study suggests that the long head of the biceps may be a greater contributor to abduction and flexion in the shoulder with cuff tear than in the normal shoulder and that sacrificing the intracapsular portion of the tendon for grafting material may not be advisable. Heikel (Heikel 1968) used fascia lata to close cuff defects and both Heikel and Bateman described the use of the coracoacromial ligament. Freeze-dried rotator cuff has been used by Neviaser and coworkers (Neviaser Neviaser 1978) In this report sixteen patients with massive tears had cadaver grafts producing decrease in nocturnal pain in all sixteen. The change in shoulder function and strength was not reported. Post (Post 1985) reported on preliminary results in five patients in whom a carbon fiber prosthesis was used to manage massive cuff deficiencies. Three had excellent to good results and two failed one because of possible infection. The author states that these results are no better than with conventional repairs. Finally synthetic cuff prostheses have been used by Ozaki and colleagues (Ozaki Fujimoto 1984) and Post. (Post 1985) The former found that of 168 shoulders with cuff tears (almost all of which were "chronic" and "massive") twenty-five could not be repaired by standard surgical techniques. Their defects were typically 6 * 5 cm. These patients had cuff reconstruction with Teflon fabric Teflon felt or Marlex mesh. This procedure was followed by a structured postoperative program including the use of an abduction orthosis to keep the arm elevated in the plane of the scapula for two to three months and continued rehabilitation for three to six months. At an average of 2.1 years follow-up 23 of 25 patients gained 120 to 160 degrees of abduction (the other 2 having had axillary nerve injury). Whereas twenty had reported continual or intolerable pain preoperatively pain was absent in twenty-three patients at follow-up. The authors found that results were better with the thicker felt and now recommend the use of 3- to 5-mm-thick Teflon felt in their patients with massive defects.
Some authors recommend postoperative immobilization in an abduction splint (Bakalim and Pasila 1975 Bateman 1963 Debeyre Patte 1965 Heikel 1968) while others advise against this. (McLaughlin 1963 Nixon and DiStefano 1975)
Results of treatment
Neer and coworkers (Neer Flatow 1988) reported the results of 233 primary cuff repairs with an average follow-up of 4.6 years. Results were excellent (essentially normal) in 77 per cent satisfactory in 14 per cent and unsatisfactory in 9 per cent. The unsatisfactory ratings were usually due to lack of strength rather than pain and usually occurred in patients with long-standing neglected tears. Hawkins and coworkers found that 86 per cent of their patients had relief of pain after repair. (Hawkins Misamore 1985) Recovery of strength was more common in patients with smaller tears. (Hawkins Misamore 1985) In other series pain relief was reported in 58 per cent (Peterson 1982) 60 per cent (Heikel 1968) 66 per cent (Debeyre Patte 1965) 74 per cent (Godsil and Linscheid 1970) and 85 per cent. (Samilson and Binder 1975)
Gore and associates (Gore Murray 1986) reviewed the results from 63 primary cuff repairs with an average of 5.5 years' follow-up. The shoulders without a traumatic onset were repaired an average of 32 months after the onset of symptoms whereas those with a traumatic onset were repaired an average of 6 months after the traumatic episode. The surgical approach and technique varied somewhat but usually consisted of acromioplasty and tendon repair to bone or to adjacent tendon. Six shoulders had biceps tendon grafts. Most shoulders were immobilized at the side for four to six weeks but twelve had immobilization in abduction. Subjective improvement was seen in 95 per cent of shoulders with repaired cuffs. Flexion averaged 126 degrees actively and 147 degrees passively. Most patients had marked relief of pain and minimal or no problems with activities of daily living. Patients with tears less than 2.5 cm long had better results than those with larger tears. The superior results with repair of smaller tears is consistent with the observations of Godsil and Linscheid (Godsil and Linscheid 1970) and Post and coworkers. (Post Silver 1983) Watson (Watson 1985) found that results were worse in patients with larger cuff defects with multiple preoperative steroid injections and with preoperative weakness of the deltoid. Ellman and colleagues (Ellman Hanker 1986) reported a 3.5-year follow-up of 50 patients having rotator cuff repair. Techniques of repair included tendon-to-tendon suture reimplantation into bone grafts and tendon flaps. Comfort and function were usually improved by these procedures. Their report provides additional support for timely repair: patients with symptoms of longer standing had larger tears and more difficult repairs. Shoulders with Grade 3 or less strength of abduction before surgery had poorer results; those with an acromiohumeral interval of 7 mm or less also had poorer results. Arthrography was not consistently accurate in estimating the size of the tear.
Hawkins found that acromioplasty and cuff repair relieved the patients' pain and restored the ability to sleep on the affected side in most patients. Seventy-eight per cent were able to use the arm above shoulder level after surgery whereas only sixteen per cent were able to do so before surgery. Hawkins and coworkers (Hawkins Misamore 1985) found that the results of cuff repair were worse in patients on Workmen's Compensation. Only two out of fourteen patients unable to work because of cuff tears could return to work after surgery whereas eight of nine patients not on Workmen's Compensation did return to work after operation. Other series of cuff repairs include those of Codman (Codman 1934b) Moseley (Moseley 1952) Neviaser (Neviaser 1971) Wolfgang (Wolfgang 1978) Bakalim and Pasila (Bakalim and Pasila 1975) Bassett and Cofield (Bassett and Cofield 1983) Earnshaw and coworkers (Earnshaw Desjardins 1982) Packer and associates (Packer Calvert 1983) Post and colleagues (Post Silver 1983) Samilson and Binder (Samilson and Binder 1975) and Weiner and Macnab. (Weiner and Macnab 1970a) Cofield (Cofield 1985) averaged the results of many reports in the literature and found that pain relief occurred in 87 per cent (range 71 to 100 per cent) and patient satisfaction averaged 77 per cent (range 72 to 82 per cent). The reader is encouraged to compare and contrast these results with those following non operative treatment which was described earlier in this chapter.
Some reports focus on the results of acute repairs. Bakalim and Pasila reviewed their series of 55 patients with arthrographically verified rupture of the cuff tendons treated surgically. (Bakalim and Pasila 1975) Whereas only half of the workers were able to return to their previous work all workers operated upon within one month of a traumatic rupture of the cuff were able to return to their jobs. Bassett and Cofield (Bassett and Cofield 1983) presented a series of 37 patients having surgical repair within three months of cuff rupture. At an average follow-up of seven years active abduction averaged 168 degrees for those having repair within 3 weeks and 129 degrees for those having repair within 6 to 12 weeks after injury. Patients with small tears averaged 148 degrees and those with large tears averaged 133 degrees of elevation. The authors concluded that surgical repair must be considered within 3 weeks of injury to obtain maximal return of shoulder function.
The importance of continued postoperative exercises is emphasized by the data of Walker and associates (Walker Couch 1987) who measured the isokinetic strength of the shoulder after cuff repair. They found a significant increase in strength between 6 and 12 months after surgery. One year after operation abduction was 80 per cent of normal and external rotation was 90 per cent of normal. Brems (Brems 1987 Jan) found that the strength of external rotation after cuff repair averaged 20 per cent at three months 38 per cent at six months 57 per cent at nine months and 71 per cent at one year.
Rokito et al (Rokito Zuckerman 1996) followed at 3 month intervals the isokinetic strength of 42 patients having repair of full thickness defects. The torques for the operated shoulder (as a percent of the opposite uninvolved shoulder) are shown in table 3).
Table 3
| Recovery of Torque After Cuff Repair [Rokito 1996 #540] | |||
| flexion | abduction | external rotation | |
| Pre operative | 54 | 45 | 64 |
| 6 months | 78 | 80 | 79 |
| 12 months | 84 | 90 | 91 |
Recovery of strength correlated primarily with the size of the tear: for small and medium sized tears the recovery of strength was almost complete during the first year. For large and massive tears recovery was slower and less consistent. The authors concluded that at least a year is required to regain strength after a cuff repair.
Kirschenbaum et al (Kirschenbaum Coyle 1993) came up with very similar results in their evaluation of 25 shoulders tested isokinetically with a pain-relieving subacromial lidocaine injection before and after cuff repair (see table 4).
Table 4
| Recovery of Torque After Cuff Repair [Kirschenbaum 1993 #521] | |||
| flexion | abduction | external-rotation | |
| Pre-operative | 33 | 37 | 36 |
| 6-months | 66 | 68 | 76 |
| 12-months | 97 | 104 | 142 |
The analysis of the results of cuff repair is hampered by lack of a uniform approach to the description of
- the shoulder's preoperative functional status
- the magnitude and location of the cuff defect
- the quality of the tissue available for repair
- the anatomical integrity at followup and
- the post operative functional status.
The need for correlation of anatomical and functional outcomes is demonstrated by the surprisingly good results obtained with debridement for irreparable cuff tears. Neer (Neer 1972) Rockwood (Rockwood 1983 and 1987) and others have reported that in certain cases when the cuff cannot be repaired comfort and function may be improved by debridement of the shreds of residual cuff and subacromial smoothing followed by muscle strengthening and range-of-motion exercises. The realization that patients may have good function and comfort in the presence of major cuff defects makes the definition of "success" after a cuff repair challenging.
Interestingly there have been few follow-up studies of the relationship of cuff integrity to the quality of the result after cuff surgery. Lundberg (Lundberg 1982) followed 21 cuff repairs with arthrography and found leakage in 7. The results in the leaking cuffs were not as good as in those with sealed cuffs. Calvert and associates (Calvert Packer 1986) performed double-contrast arthrograms in 20 patients at an average of 30 months after operative repair of a torn cuff. In 17 of 20 shoulders the contrast leaked into the bursa indicating a cuff defect. These defects were estimated to be small in 8 medium in 8 and large in 2. However 17 patients had complete relief of pain 15 had a full range of shoulder elevation and 10 felt that they had regained full function. The authors suggest that a complete closure of the cuff is not essential for a good functional result and that arthrography may not be helpful in the investigation of failure of repair.
Ultrasonography appears to offer a greater potential for evaluating postoperative cuff integrity. Mack and coworkers (Mack Nuberg 1987) investigated the accuracy of ultrasonography in this regard. In a group of symptomatic postoperative shoulders that were subsequently reoperated ultrasonography accurately diagnosed recurrent cuff tears in 25 of 25 cases and correctly confirmed cuff integrity in 10 of 11. Using expert ultrasonography Harryman (Harryman Mack 1991) correlated the integrity of the cuff with functional status following 105 surgical repairs of chronic rotator cuff tears in 89 patients at an average of five years postoperatively. The patients' ages at the time of repair averaged 60 years (range 32 to 80). The numbers of patients in each age decade were as follows: 30-39:l 40-49:16 50-59:31 60-69:42 70-79:14 and 80-89:1. Eighty-six (82%) of the shoulders had no prior attempt at repair of the cuff.
In all of the surgeries an anterior-inferior acromioplasty was carried out. The involved tendon or tendons were mobilized as necessary. A bony trough was created in the humerus to reattach the mobilized tendons. The site of reattachment was usually in the sulcus adjacent to the humeral articular surface. In some cases the trough was placed somewhat more medially if after mobilization the tendons did not reach their original anatomic attachment without undue tension when the arm was at the side. The cuff was protected from active use for three months postoperatively.
The status of the cuff at surgery and at follow-up was characterizedin terms of the integrity of the different tendons: Type O was a cuff of normally full thickness Type 1A was thinning or a partial-thickness defect of the supraspinatus tendon Type 1B was a full-thickness defect of the supraspinatus Type 2 wasa full thickness two-tendon defect involving the supraspinatus and the infraspinatus and Type 3 was a full-thickness defect involving three tendons: the supraspinatus infraspinatus and subscapularis.
The results are summarized in table 5.
Table 5
Integrity of Cuff Repairs at Follow-up
| Size of Cuff Defect at Followup Examination | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Size of Defect Repaired at Surgery | Primary Repairs | Repeat Repairs | Total No. Repairs | None (0) | Partial (1A) | Supraspinatus Tear (1B) | Supraspinatus Infraspinatus Tear (2) | Supraspinatus Infraspinatus Subscapularis tear (3) | Percent Intact (0 or 1A) | Years Followup Average & Range |
| All Cases | 86 | 19 | 105 | 40 | 28 | 12 | 14 | 11 | 65% | 5 (2-11) |
| Partial Tears (1A) | 5 | 1 | 6 | 4 | 2 | 0 | 0 | 0 | 100% | 2.7 (2-6) |
| Supraspinatus Tears (1B) | 39 | 10 | 49 | 23 | 16 | 3 | 5 | 2 | 80% | 5.1 (2-10.5) |
| Supraspinatus & infraspinatus (2) | 25 | 3 | 28 | 7 | 9 | 6 | 5 | 1 | 57% | 5.9 (2-6) |
| Supraspinatus infraspinatus & subscapularis (3) | 17 | 5 | 22 | 6 | 1 | 3 | 4 | 8 | 32% | 4.1 (2-11) |
| Intact at Follow-up | 60 | 8 | 68 | |||||||
(Reproduced with permission from Matsen FA III et al: Practical Evaluation and Management of the Shoulder. W.B. Saunders Company Philadelphia PA 1994.)
No patient who had a partial thickness tear repaired had a full thickness retear. In 80 percent of shoulders with repaired full-thickness supraspinatus tears the cuff was found to be intact (no full thickness defect) at follow-up. Only 57 percent of cuffs that had tears involving both the supraspinatus and infraspinatus were intact at an average follow-up of six years. Less than one-third of the cuffs which had tears involving all three major tendons were intact after repair at an average of four years of follow-up.
Patients were generally satisfied with the results of surgery even when expert sonography showed that the cuff was no longer intact (see table 6).
Table 6
Influence of Size of Cuff Defect at Follow-up on Active Range Comfort
and Satisfaction at Follow-up
Active Range of Motion at Follow-up
| Size of Cuff Defect at Followup | Number | Flexion | External Rotation at side | External Rotation at 90 Abduction | Internal Rotation | Total Painless | Total Satisfied |
| None (0) | 40 | 132 | 41 | 71 | T7 | 37 | 39 |
| Partial (1A) | 28 | 124 | 38 | 68 | T7 | 21 | 23 |
| Supraspinatus (1B) | 12 | 107 | 34 | 63 | T8 | 8 | 12 |
| Supraspinatus Infraspinatus (2) | 14 | 109 | 25 | 48 | T9 | 10 | 10 |
| Supraspinatus Infraspinatus Subscapularis (3) | 11 | 71 | 27 | 61 | T10 | 8 | 10 |
| Total | 105 | 84 | 94 |
(Reproduced with permission from Matsen FA III et al: Practical Evaluation and Management of the Shoulder. W.B. Saunders Company Philadelphia PA 1994.)
Follow-up
Shoulders with intact repairs (no full thickness defect) at follow-up had the greatest range of active flexion (129±20 degrees) as compared to those with large recurrent defects (71±41 degrees) (see figure 53).Shoulders with intact repairs also demonstrated the best function in activities of daily living. Where the cuff was not intact the degree of functional loss was related to the size of the recurrent defect (see figure 54).
Although the chances of having an intact repair at followup was less for those with large tears patients with intact repairs of large tears had just as good function as did those with intact repairs of small tears. Similarly there was an overall greater incidence of recurrent defects in shoulders with repeat repairs yet shoulders with intact cuffs after repeat repairs functioned as well as did those with intact primary repairs.
From this study it can be concluded that
- the integrity of the rotator cuff at follow-up (and not the size of the tear at the time of repair) is a major determinant of the functional outcome of surgical repair
- that the chances of the repair of a large tear remaining intact however are not as good as those for a small tear and
- that older patients tended to have larger tears and to have a higher incidence of recurrent defects (see table 7).
Table 7
Influence of Size of Cuff Tear Repaired at Surgery
on Active Range of Motion at Follow-up
| Size of Defect Repaired at Surgery | Number | Age at Repair (means ±s.d.) | Flexion | External Rotation at side | External Rotation at 90 Abduction | Internal Rotation |
| Partial (1A) | 6 | 49±13 | 126_ | 38_ | 68_ | T8 |
| Supraspinatus (1B) | 49 | 57±8 | 129_ | 40_ | 70_ | T7 |
| Supraspinatus Infraspinatus (2) | 28 | 64±8 | 119_ | 28_Ü | 60_ | T8 |
| Supraspinatus Infraspinatus Subscapularis (3) | 22 | 64±8 | 92_Ü | 33_ | 60_ | T10_Ü |
(Reproduced with permission from Matsen FA III et al: Practical Evaluation and Management of the Shoulder. W.B. Saunders Company Philadelphia PA 1994.)
In a very comparable study Gazielly et al (Gazielly Gleyze 1994 Gazielly Gleyze 1995a Gazielly Gleyze 1995b) examined the anatomic condition by ultrasonography and the function of the rotator cuff at four years following surgical repair in a series of 100 full thickness rotator cuff tears. The series comprised 98 patients (62 men and 36 women) whose average age was 56 years. 69 tears were less than 2 cm in size (39 cases) or between 2 to 4 cm (3 cases) of the supra-spinatus 22 tears of the supra- and infraspinatus measuring between 2 to 4 cm and 9 massive tears. All 98 patients were operated on by the same surgeon using the same repair technique. Ultrasonography revealed intact cuffs in 65 per cent thinned cuffs in 11 per cent and recurrent full thickness tears in 24 percent of cases. The risk of recurrent tear increased with the extent of the tear to be repaired (57 percent) in older patient (25 percent) and with a higher level of post-surgical occupational use (18 percent). At follow-up they noted a close correlation between the anatomic condition of the cuff by ultrasound and Constant's functional score.
Similar results have been reported by Cammerer et al (Cammerer Habermeyer 1992) and Bellumore et al. (Bellumore Mansat 1994)
Wulker et al (Wulker Melzer 1991) followed 97 of 116 shoulders operated on for rotator cuff lesions after an average follow-up time of 37 months. Seventy percent had a good or excellent clinical result however ultrasonographic examination revealed that only 37 had a normal rotator cuff 31 had thinning and/or hyperdensity and 29 had a complete rupture of the cuff. The authors concluded that rotator cuff tears should be closed only if this can be achieved without undue tension and without extensive tissue mobilization or coverage otherwise they recommended that the lesion should be debrided and left open and only an anterior acromioplasty should be performed.
Taken together these studies provide strong evidence that following cuff repair surgery a high percentage of patients have a satisfactory clinical result in spite of recurrence of the cuff defect. Several conclusions are evident:
- one cannot infer integrity of the repaired cuff from a "good" or "excellent" clinical result
- factors other than cuff integrity must contribute to the quality of the clinical result from rotator cuff surgery and
- if we are to learn more about the value of cuff repair analysis of cuff integrity and change in functional status must become essential elements in outcome studies of cuff repair surgery.
Arthroscopically assisted repair
Some authors have reported short term follow-up of arthroscopic assisted rotator cuff repair. (Levy Urie 1990 Palette Warner 1993) These authors suggest that required components of the repair include an adequate smoothing of the undersurface of the acromion and the AC joint; arthroscopic (or open) resection of the distal clavicle in the presence of significant AC joint arthrosis; mobilization of the entire rotator cuff with release of adhesions and scar tissue; and repair of strong tendon to a properly placed well-prepared bleeding bone trough.
The rotator cuff repair is often performed through a lateral deltoid muscle splitting incision. The deltoid is not detached from the acromion. The deltoid muscle is split with blunt dissection with careful attention to the axillary nerve which crosses on the deep surface of the deltoid as close as 5 cm to the lateral edge of the acromion. A bony trough is developed in the greater tuberosity. Reapposition of the torn cuff edge to the greater tuberosity is accomplished with nonabsorbable sutures passed through drill holes and tied over bone.
Alternative methods for arthroscopically assisted cuff repair include the percutaneous insertion of absorbable tacks and metallic staples. Use of fixation implants of this type carries the potential for loss of fixation particularly in patients with soft cancellous bone. Loss of fixation can result in failure of tendon repair as well as mechanical irritation caused by displacement of these devices in the subacromial space.
Palette et al reported success in the arthroscopic management of small tears. (Palette Warner 1993) Levy et al (Levy Urie 1990) in 1990 reported on 25 patients with full thickness rotator cuff tears treated with an arthroscopically assisted rotator cuff repair. After performing an arthroscopic acromioplasty the rotator cuff was identified debrided mobilized with arthroscopically placed sutures and then repaired to a bony trough through a limited deltoid splitting approach. The patients average age 57.7 years (range 21-74 years) were evaluated at an average of 18 months (range of 12-27 months). Based on the UCLA shoulder rating scale 80 percent of the patients were rated as excellent or good with reported significant improvements in pain function motion and strength. Ninety-six per cent of the patients were satisfied with their result. Of the 15 large tears (3-5 cm) four were excellent 6 were good (67% satisfactory) four were fair and one was poor (33% unsatisfactory). Of the patients with small (< 1 cm) or moderate (1-3 cm) size tears 100% received a satisfactory rating.
Warren et al (Warren Altchek 1991) reported good or excellent results in 13 of their 17 patients who underwent arthroscopic acromioplasty and arthroscopic-assisted rotator cuff repair who were followed for a minimum of two years with an average follow-up of 25 months. Tear size was small in 4 moderate in 5 large in 6 and massive in 2. The rotator cuff was repaired into a prepared bony trough using arthroscopically placed sutures through a limited deltoid splitting incision and in some cases using percutaneous fixation with a cannulated tack. Eight of nine tennis-players and all the golfers returned to their previous sports.
Paulos and Kody (Paulos and Kody 1994) in 1994 reported their results of 18 consecutive patients who underwent arthroscopic acromioplasty and rotator cuff repair through a 4 cm deltoid-splitting approach with an average follow-up of 46 months (range 36-72 months); mean age 47.2 years (range 26-74 years). Sixteen repairs were tendon-to-bone; two repairs were tendon-to-tendon. Sixteen patients (88%) scored good to excellent on the UCLA shoulder rating scale with significant improvement in pain and function scores. Two patients had poor results; both had workers compensation cases pending. One patient with a poor result had 2 complications: superficial infection and failure of repair that required reoperation. 17 of the 18 patients (94%) were satisfied with their result.
In 1994 Liu (Liu 1994) reported on 44 patients (average age 58 years range 35-76) with full thickness rotator cuff tears at an average of 4.2 years (range 2.5 - 6.1 years) after arthroscopic assisted rotator cuff repair. Eighty-five percent of the patients were discharged from the hospital immediately after the operation. The results were rated as good or satisfactory in 84% (37/44) (8/8 in those with small tears (less than 1 cm) 15/17 with moderate tears (1 to 3 cm) 12/15 with large tears (3 to 5 cm) and 2/5 with massive tears (greater than 5 cm). Eighty-eight percent of the patients were satisfied with the result and 64% of the athletes returned to their previous sport. The size of the tear seemed to be a determining factor in the functional outcome: the small and moderate tears did better than large and massive tears. The patients satisfaction however did not seem to relate to the size of the tear repair; those with small moderate and large tears were equally satisfied.
In 1995 Baker and Liu (Baker and Liu 1995) compared the results of open and arthroscopically assisted rotator cuff repair in 36 patients with a minimum follow-up of 2 years. The open repair group (average age 60 years) comprised 20 shoulders with an average follow-up of 3.3 years; the arthroscopic assisted repair group (average age 59 years) comprised 17 shoulders with an average follow-up of 3.2 years. Overall the open repair group had 88 percent good-to-excellent results and 88 percent patient satisfaction; the arthroscopically assisted repair group had 85 percent good-to-excellent and 92 percent patient satisfaction (based on the UCLA rating scale). The functional outcome with regard to shoulder flexion strength of abduction and the size of the rotator cuff tear repaired did not differ significantly between the two treatment groups. In general however small and moderate sized tears (< 3 cm) demonstrated earlier return to full function after arthroscopically assisted rotator cuff repair; this group was hospitalized 1.2 days less and returned to previous activities an average of 1 month earlier. In the patients with large tears 2 out of 4 patients (50%) in the arthroscopically assisted repair group and 4 of 5 (80%) in the open repair group had good-to-excellent results. In general the authors found arthroscopically assisted rotator cuff repair to be as effective as open repair in the treatment of small and moderated sized tears (<3 cm), whereas large tears did better after open repair.
These studies suggest that arthroscopic acromioplasty combined with arthroscopically-assisted rotator cuff repair can provide acceptable clinical results in the management of small full thickness rotator cuff tears in the presence of excellent quality tissue with minimal tissue retraction and scarring. These results however are not directly comparable with the results of traditional open surgery because studies involving open techniques include larger numbers of older patients many of whom have large chronic tears requiring extensive soft-tissue mobilization. The long term clinical results and the integrity of the cuff after these arthroscopically-assisted repairs have yet to be determined.
Open operative treatment when repair is not possible
While it used to be said by some that "the term irreparable cuff reflects more on the surgeon than the patient the fact is that some rotator cuff tears may be impossible to repair. Rockwood et al (Rockwood, 1983 and 1987, Rockwood, Williams, 1995) reported on their experience using a modified Neer acromioplasty and debridement of massive irreparable lesions involving the supraspinatus and infraspinatus tendons in 53 shoulders (average age 60). At an average of 6.5 years followup the comfort, function and satisfaction were satisfactory in 83%. Good prognostic findings were an intact biceps, an intact anterior deltoid and no previous shoulder surgery. Active forward flexion improved from 105 to 140 degrees. These results indicate that subacromial smoothness and vigorous post surgical rehabilitation can substantially improve comfort and function, even when large cuff defects are irreparable.
In a small series Hawkins et al (Hawkins, Misamore, 1985) reported only 50 percent satisfactory results with open subacromial decompression alone in patients with massive full thickness rotator cuff tears.
Bakalim and Pasila (Bakalim and Pasila, 1975) found that acromial excision alone gave relief of night pain in certain cases.
Arthroscopic operative treatment when repair is not possible
Several authors have reported acceptable clinical results with full thickness cuff defects when arthroscopic acromioplasty and debridement was performed without rotator cuff repair, especially for the sedentary, low demand patients whose main complaint is pain. (Ellman, 1988, Esch, Ozerkis, 1988, Gartsman, 1990, Hawkins, Saddamis, 1992, Speer, Lohnes, 1991, van Holsbeeck, DeRycke, 1992)
In one of the earliest studies, Wiley (Wiley, 1985), in 1985, reported on 20 patients with full thickness rotator cuff tears who underwent arthroscopic, rotator cuff debridement and shoulder manipulation without acromioplasty. Within 24 months, sixteen patients had pain relief (5 complete, 11 partial), twelve had increased range of motion, and 11 were able to return to work. He concluded that arthroscopic treatment was useful in treating older patients with chronic shoulder pain associated with full thickness rotator cuff tears.
Ellman (Ellman, 1987) in 1987, presented 10 patients with full thickness tears of the rotator cuff treated with arthroscopic acromioplasty and rotator cuff debridement. Based on the UCLA shoulder rating scale, 80% were rated satisfactory (8 good) and 20% unsatisfactory (2 poor). It was noted that none of the eight satisfactory results achieved an excellent objective rating.
Esch et al (Esch, Ozerkis, 1988), in 1988, presented their results according to the degree of rotator cuff tendon failure. Their patients with complete tears were divided into groups of tears less than 1 cm in size, tears greater than 1 cm in size, and massive tears. The patients were treated with an arthroscopic acromioplasty, coracoacromial ligament resection, and debridement of acromioclavicular spurs. All patients were followed for a minimum of 1 year. Four patients with tears less than 1 cm in size had a satisfactory result and an excellent rating. Of the 16 patients with tears greater than 1 cm in size, 14 were satisfied and objectively 13 had a good or excellent result (based on the UCLA shoulder rating scale). There were three fair objective ratings and no poor ratings. Of the 6 patients with massive tears, 5 were satisfied but only 3 had a satisfactory score. Thus, patients with complete rotator cuff tears had an overall patient satisfaction rate of 88% and an objective satisfactory rating of 77%. Esch subsequently concluded that results are related to tear size. Patients with small full thickness tears may achieve excellent results with arthroscopic acromioplasty and cuff debridement. Of the patients with large tears, only 4 of the 13 obtained an excellent objective result.
Gartsman (Gartsman, 1990), as part of a larger series, reported on 25 patients with full thickness rotator cuff tears treated with arthroscopic acromioplasty, resection of the coracoacromial ligament and subacromial bursa, removal of osteophytes, and a minimal debridement of the rotator cuff defect. The tears were divided into four groups based on size of the tear; small tears of less than 1 cm (3 total), tears between 1 cm and 3 cm (13 total), tears between 3 cm and 5 cm (6 total) and 3 massive tears which were greater than 5 cm. At an average of 31 months, there were 14 satisfactory and 11 unsatisfactory results. Seven of these patients were subsequently treated with open rotator cuff repair, six of which had a satisfactory result. Notably, there was no correlation between the final result and the patient's age, sex, hand dominance, or the location of the tear. Only rotator cuff tear size correlated with outcome - 13 of 16 patients with a tear less than 3 cm in size had a satisfactory result while only 1 of 9 patients with a larger tear (over 3 cm) did well.
Montgomery et al (Montgomery, Yerger, 1992) reported on 87 patients with 89 full thickness rotator cuff tears who failed to respond to conservative treatment. Fifty patients (Group I) were treated with open rotator cuff repair and Neer acromioplasty. Thirty-eight patients (Group II) were managed by arthroscopic debridement, acromioplasty, and abrasion of the greater tuberosity. With similar size rotator cuff tears represented in each group at 1 year follow-up, the authors found no statistically significant difference between the two groups. However, on re-evaluation at 2 years post-surgery, the open surgical repair group (I) was statistically much better than the arthroscopic debridement group (II)with regard to pain and function. Four of the 38 patients in the arthroscopic debridement group developed rotator cuff tear arthropathy which was thought to occur secondary to the instability and abnormal movement of the humeral head on the glenoid.
In 1991, Levy et al (Levy, Gardner, 1991) reported on 25 patients with full thickness tears of the rotator cuff treated with arthroscopic acromioplasty and rotator cuff tendon debridement alone. There was significant improvement in pain, function, motion, and strength. 84% of the cases were rated as excellent or good (and 88% of the patients were satisfied with the procedure). Although all tear sizes were improved significantly, small tears fared better than larger tears.
In a follow-up series (Zvijac, Levy, 1994), Zvijac, Levy and Lemak reevaluated all 25 patients from the original study group with full thickness rotator cuff tears who underwent arthroscopic acromioplasty. At mean follow-up of 45.8 months, 68% of the patients were rated as excellent or good, representing a significant decrease from the initial report of 84% satisfactory result at a mean follow-up of 24.6 months. The authors found a significant decrease in rating with regard to pain and function. Ratings for motion and strength did not change significantly with time. Large and massive rotator cuff tears fared worse over time when compared to small and moderate size tears. These finding led the authors to abandon support for the use of arthroscopic acromioplasty and rotator cuff debridement alone in the treatment of repairable full thickness rotator cuff tears.
In 1993, Ellman et al (Ellman, Kay, 1993) reported their follow-up results of 40 full thickness rotator cuff tears treated by arthroscopic acromioplasty and debridement in a selected group of patients. The patients were divided into 3 groups based on the size of their tear. Small (0-2 cm) tears (N=10) in older patients not involved in strenuous activities were rated satisfactory in 90% of cases. Patients with larger (2-4 cm) repairable tears (N=8) did poorly (50% satisfactory results). Arthroscopic treatment in patients with massive irreparable tears (N=22) did not improve range of motion or restore strength, but did result in significant pain relief and 86% were satisfied with the results on a limited-goals basis". Ellman and his co-authors concluded that for patients with medium-size tears pain relief from arthroscopic acromioplasty alone is inadequate and the "procedure probably should not be offered". In carefully selected patients described as "relatively older and very sedentary" however with small rotator cuff tears (0-2 cm) arthroscopic acromioplasty can have a useful role. Ellman emphasized that even for these patients and certainly for the majority of patients repairable rotator cuff tears are best treated with open surgical repair.
In a series of 80 consecutive arthroscopic acromioplasties in 76 patients with stage II and III impingement syndrome Paulos et al (Paulos and Franklin 1990) identified seven patients with full thickness rotator cuff tears. Three of these patients all with small (1 cm) tears remained symptomatic and required reoperation for open repair of the rotator cuff tear.
In 1993 Oglivie-Harris et al (Ogilvie-Harris and Demaziere 1993) in a prospective cohort study compared the results of arthroscopic acromioplasty and rotator cuff debridement (22 patients) and open repair and acromioplasty (23 patients) as treatment for tears of the rotator cuff 1 to 4 cm in size. Follow-up varied from 2 to 5 years. The two treatment groups showed no significant differences in age size of tear preoperative pain function range of active forward flexion and strength of forward flexion. At follow-up both groups had similar pain relief and range of active forward flexion. The open repair group scored significantly better for function strength and overall score however patient satisfaction was similar in both groups. These authors found no significant difference in the final result in relation to the age of the patient or the size of the rotator cuff tears. On the basis of their results the authors consider use of arthroscopic acromioplasty and debridement for patients with demands whose main complaints are pain and loss of range of movement. For patients however who needs good function and strength arthroscopic debridement and acromioplasty are not sufficient and open repair and acromioplasty is advised.
Olsewski and Depew (Olsewski and Depew 1994) in 1994 reported on their results of arthroscopic acromioplasty and rotator cuff debridement performed on 61 consecutive patients with a minimum of 2 year follow-up (mean 27.7 months). In this study 13 full thickness rotator cuff tears were identified. Of the 13 full-thickness tears treated 10 were rated satisfactory (77%) and 3 unsatisfactory (33%). Of the 10 satisfactory results eight were in patients who were either retired or worked at sedentary jobs that did not demand above shoulder activities and strength and whose principal preoperative complaint was pain. All 10 of these patients had relief of their pain. The 3 unsatisfactory results were all in active patients with demands on strength and overhead activity.
Burkhart (Burkhart 1991) described 10 patients with massive (irreparable/ greater than 5 cm) complete rotator cuff tears involving primarily the supraspinatus treated with arthroscopic acromioplasty with debridement of redundant nonfunctional rotator cuff tissue. All patients except one had normal active motion and strength preoperatively and all had a roentgenographically normal acromiohumeral distance and an anterior-inferior acromial osteophyte. The procedure was offered to a subset of older patients with activity limiting pain who were preoperatively found to have a full range of active shoulder motion and normal strength of external rotation. Arthroscopic debridement and decompression was accompanied by pain relief without loss of motion or strength in all 10 patients. The follow-up period ranged from eight to 33 months (mean 17.6 months). Patients ranged from 53 to 77 years of age (average 65 years). There were 7 excellent and 3 good results. All patients were satisfied with their results.
Cost effectiveness of treatment of full thickness cuff tears
Rotator cuff disease is one of the commonest afflictions of the shoulder. Many health care dollars are spent on its evaluation and management. It is apparent that a large number of variables affect the effectiveness of treatment of cuff lesions. The cost of various treatment methods varies substantially as well. To initiate a practical investigative method by which the cost effectiveness might be compared among treatment methods the authors conducted a preliminary study of 67 unmatched patients presenting for treatment of documented symptomatic full thickness tears. Based on our clinical assessment and the desires of the patient one of three treatment methods was selected for each patient: nonoperative management subacromial smoothing without repair and surgical repair. The number of patients average age gender and length of follow-up for the patients in each of the three groups is given in table 8.
Table 8
Data on 67 Patients Treated for Documented Full Thickness Tears of the Rotator Cuff
| Number of patients | Average age | Percent female | Average followup (yrs) | |
| Nonoperative | 36 | 62.4 | 36 | 1.7 |
| Subacromial Smoothing | 11 | 67.8 | 45 | 1.7 |
| Cuff repair | 20 | 60.3 | 10 | 2.0 |
SST and SF-36
All patients completed Simple Shoulder Tests and SF-36 questionnaires preoperatively and at follow-up. The effectiveness of treatment was measured in terms of the postoperative-preoperative change in the number of "yes" responses on the Simple Shoulder Test and the postoperative - preoperative change in the SF 36 comfort score. This analysis indicated that the greatest improvement was found in the group having surgical repair (see solid bars in figure 55). The change in SST and SF 36 comfort score results for each patient were then divided by the total hospital office and physician charges for the treatment to yield the average change/$1000 charge. In this analysis nonoperative treatment was associated with the greatest change per unit charge (see hollow bars in figure 55).
While no conclusions should be drawn from these preliminary results it is hoped that further studies of this type will help determine the cost-effectiveness of different treatment methods.
Authors' preferred method of treatment for surgical management of full thickness rotator cuff tears
The goal of rotator cuff surgery is to improve comfort and function of the shoulder. Surgery is considered
- in the patient with a significant acute cuff tear and
- in the patient with a chronic cuff defect associated with significant symptoms which have been refractory to a 3 month course of nonoperative management.
In the situation of an acute cuff tear in a previously normal shoulder the quality and quantity of tendon for repair should be excellent. Repair should be carried out promptly before tissue loss retraction and atrophy occur.
For tears older than six months surgical repair is not an emergency: there is time to explore nonoperative management including a general shoulder stretching and strengthening program. This nonoperative program may be the treatment of choice in patients with chronic weakness who are not candidates for surgery or for those in whom achieving a durable repair seems unlikely (see table 2).
This regime has been described earlier in this chapter as the "Jackin's program"; it emphasizes stretching and strengthening the muscle groups which provide elevation and rotation of the shoulder. Surgical exploration is considered for patients with functionally significant symptoms from longer-standing tears refractory to nonoperative management provided that their expectations are realistic. While a successful cuff repair may increase the strength of the shoulder patients with repairs of chronic tears are advised against returning to heavy lifting pushing pulling or overhead work after surgery for fear of re rupturing the abnormal tendon tissue. Thus we initiate vocational rehabilitation as soon as the diagnosis is made indicating that in spite of optimal treatment there is a substantial risk of retearing if the cuff is again subjected to major loads. It is important to remind both the patient and the employer that a cuff tear usually occurs through abnormal cuff tendon. Repairing the tear does not restore the quality of the tendon tissue; thus the repaired cuff remains permanently vulnerable to sudden or large loads.
Critical determinants of a durable repair are the quality of the tendon and muscle and the amount of cuff tendon tissue that has been lost. The strength of the cuff tendon diminishes with age and disuse; as a result the chances of a durable cuff repair also decrease in older and less active shoulders. This is particularly the case if the cuff defect has been long-standing.
Table 2 lists some of the factors that contribute to a durable repair as well as those which predispose to failure. None of the factors in this table requires special imaging of the rotator cuff; all are discernible from the history physical examination and plain radiographs. While none of these factors is a contraindication to surgery each works to some degree against the chances of a durable repair. The choice of treatment of shoulder weakness caused by cuff failure is determined by the functional needs of the patient and the likeliness of a durable surgical repair. Patients with low functional requirements and a substantial number of the "discouraging" factors from table 2 are given a nonoperative program to help optimize the strength and coordination of the muscles about the shoulder that remain intact. At the opposite extreme patients with major functional demands and mostly "encouraging" factors are presented with the option of an attempt at surgical repair and informed that the success of this repair will be determined primarily by the quality of the tendon and muscle and the amount of tissue lost.
We recall that cuff repair is a shoulder tightening operation: in a sense it is a capsulorrhaphy. Thus it is not a treatment for the shoulder whose primary functional limitation is caused by tightness even if a cuff defect is also present. If the shoulder demonstrates stiffness a shoulder mobilization program is instituted before consideration of surgery.
About the surgery
For surgery the patient is positioned in a semi-sitting (beach chair) position. Both the anterior and posterior aspects of the chest and the arm are prepared to allow access to the back of the shoulder and full motion of the arm. Surgery begins with an inspection of the cuff through a "deltoid on" acromioplasty approach (see figure 56). This incision offers excellent exposure and the opportunity for a cosmetic closure. Great care is taken to preserve the tendon fibers of the deltoid origin to permit a strong repair. The deltoid has an important tendon of origin between its anterior and middle thirds. Arising from the anterior lateral corner of the acromion this tendon is not only the guide to exposure of the cuff but is also the key to reattachment of the deltoid origin at the conclusion of the surgery. This tendon is split longitudinally for 2 cm distal to the acromion in line with its fibers taking care to leave some of the tendon on each side of the split. The split is continued up over the acromion and into the trapezius insertion. Although it is usually unnecessary for inspection of the cuff additional exposure can be achieved by sharply dissecting the deltoid origin off the acromion for one centimeter on either side of this split so that the strong bony attachment fibers remain with the muscle. These fibers provide a strong "handle" on the muscle so a solid repair can be achieved at the conclusion of the procedure. Splitting the parietal layer of the bursa on the deep aspect of the deltoid provides a view of the rotator cuff. Later closure of the split is facilitated if at this point in the procedure a suture is placed on each side of the split fixing the incised bursal layer to the deltoid.
Before a "reflex" acromioplasty is performed this window is used to inspect the cuff and determine its reparability without further compromising the deltoid or the coracoacromial arch. Hypertrophic bursa and scar tissue are resected to allow a good view of the cuff tendon involvement tendon quality and tendon tissue loss. Cuff tendon involvement is conveniently characterized using the system introduced by Harryman et al (Harryman Mack 1991) which is based on the number of tendons torn. In Type 1 only one tendon (almost always the supraspinatus) is torn. In Type 2 two tendons (usually the supraspinatus and infraspinatus) are torn. In Type 3 the supraspinatus infraspinatus and subscapularis are torn. Type 1 is broken down into Type 1A-a partial thickness-tear and Type 1B-the full thickness tear confined to a single tendon. The quality of the cuff tissue is judged in terms of its ability to hold a strong pull applied to a suture passed through its edge. Finally it is critical to note the amount of tissue that has been lost. The extent of tissue loss and the ability of the remaining tissue to hold suture are the major determinants of cuff reparability.
Standard anteroinferior acromioplasty
If inspection of the cuff at surgery reveals good quality tissue in sufficient quantity and quality for a robust repair a standard anteroinferior acromioplasty may be performed if necessary to improve exposure and to protect the repair from abrasion. A flexible osteotome is directed so that the anterior undersurface of the acromion is resected in the same plane as the posterior acromion (see figure 57). Rough spots are smoothed with a motorized bur.
The goal of repair is a strong fixation of the tendon to the humerus under normal tension with the arm at the side. The desired attachment site is at the sulcus near the base of the tuberosity. This goal is facilitated by using three stages of sequential release. These releases are required because the cuff is usually retracted and because tissue is lost in chronic cuff disease. Unless these releases are carried out increased tension in the repaired tendon will predispose to tightness of the glenohumeral joint and will additionally challenge the repair site. (Zuckerman Leblanc 1991) The humeral head is rotated to present successively the margins of the cuff defect through the incision rather than enlarging the exposure to show the entire lesion at one time. The deep surface of the cuff is searched for retracted laminations. All layers of the cuff are assembled and tagged with sutures. By applying traction to these sutures the cuff is mobilized sequentially as necessary to allow the torn tendon edge to reach the desired insertion at the base of the tuberosity. First the humeroscapular motion interface (see figures 58 and 59) is freed between the cuff and the deltoid acromion coracoacromial ligaments coracoid and coracoid muscles. Next the coracohumeral ligament/rotator interval capsule (see figure 60) is sectioned around the coracoid process to eliminate any restriction to the excursion of the cuff tendons and to minimize tension on the repair during passive movement (see figure 61). This release of the coracohumeral ligament and rotator interval capsule also contributes to the comfort and ease of motion after the surgical repair by minimizing the capsular tightening effect of cuff repair. (Zuckerman Leblanc 1991) At this point the ease with which the cuff margins can be approximated to their anatomic insertion at the base of the tuberosity is evaluated. If good tissue cannot reach the sulcus the third release is carried out. This release divides the capsule from the glenoid just outside the glenoid labrum (see figure 52) which allows the capsule and tendon of the cuff to be drawn further laterally toward the desired tuberosity insertion without restricting range of motion.
After the necessary releases have been completed a judgment is made concerning the site at which the cuff can be implanted into the bone without undue tension while the arm is at the side. Ideally the site of implantation will be in the sulcus at the base of the tuberosity. In large cuff defects a somewhat more medial insertion site may be necessary. Often when a medial insertion site is required for a large cuff defect the new insertion lies in an area where the articular cartilage has been damaged by abrasion against the undersurface of the acromion.
The repair is accomplished as a tongue in groove with the cuff tendon drawn into a trough near the tuberosity providing a smooth upper surface to glide beneath the acromion (see figure 62). This groove provides the additional advantage that if some slippage occurs in the suture fixation of the cuff to bone contact between these two structures is not lost. Nonabsorbable sutures woven through the tendon margin are passed through drill holes in the distal tuberosity so that the knots will not catch beneath the acromion (see figure 63). The knots are tied over the tuberosities so that they will lie out of the subacromial space. If the bone of the tuberosities is osteopenic the sutures can be passed through bone more distally even down to the junction of the metaphysis and diaphysis. If there is a longitudinal component to the tear it is repaired side-to-side with the knots buried out of the humeroscapular motion interface. The repair is checked throughout a range of motion to 140 degrees of elevation and 40 degrees of external rotation to assure that it is strong that it is not under excessive tension and that it will permit smooth subacromial motion. If additional subacromial smoothing is required to allow smooth passage of the repaired tendon it is performed at this time.
After a careful and robust deltoid repair using nonabsorbable sutures (see figure 64) and cosmetic skin closure the patient is returned to the recovery room with the affected arm in continuous passive motion (see figure 65). Immediate postoperative motion is valuable because there is a tendency for scarring between the raw undersurface of the acromion and the upper aspect of the rotator cuff or proximal humerus. Immediate postoperative continuous passive motion is facilitated if the surgery is performed under a brachial plexus block which lasts up to 18 hours after surgery. Continuous passive motion is continued for up to 48 hours after surgery but does not appear to be necessary after that. The patient is expected to perform passive exercises in flexion and external rotation. Before discharge from the medical center the patient should be able to attain comfortably 140 degrees of passive flexion and 40 degrees of passive external rotation. A progress chart mounted on the patient's wall helps to document progress toward these discharge goals (see figure 66).
Post discharge management must consider the magnitude of the tear and the strength of the repair. It is unlikely that the repair will have substantial strength until at least three months after surgery. (Frank 1996) As is the case with repairs of the anterior cruciate ligament major cuff repairs may require six to twelve months to regain useful strength. Thus in the first several postoperative months the emphasis is placed on maintaining passive motion and avoiding loading of the repair. Posterior capsular stretching is not started until three months after surgery. Gentle progressive strengthening of the repaired cuff muscles is also started at three months. Work and sports are not resumed until the shoulder is comfortable flexible and strong.
When cuff repair cannot be achieved
If the initial inspection of the cuff reveals major tissue loss and residual tendon of poor quality and if it becomes evident that a robust repair cannot be performed the coracoacromial arch is preserved. When primary stability from an intact cuff cannot be restored it is important to avoid a "reflex" acromioplasty. Sacrifice of the coracoacromial arch jeopardizes the secondary stabilization required in cuff deficiency. Without this secondary restraint the shoulder is prone to anterosuperior "escape" of the humeral head when superiorly directed loads are applied to the humerus. Therefore when a strong rotator cuff repair cannot be performed because of limited quantity and quality of the residual cuff tissue we preserve the coracoacromial arch and assure the smoothness of its undersurface to allow unimpeded passage of the humeral head and residual cuff beneath. Any debris scar useless fronds of cuff or thickened bursa in the subacromial area is excised. It is important to also assure smoothness of the upper surface of the uncovered proximal humerus particularly if the tuberosities are prominent or irregular.
A strong repair of the deltoid is accomplished using a side-to-side repair of the surgical split in the deltoid tendon and a secure reattachment to the acromion using drill holes in the bone as necessary (see figure 64). The full thickness of the deltoid including the deltoid side of the bursa is incorporated in the sutures to be certain that it does not impede smooth motion in the humeroscapular motion interface.
A subcuticular skin closure reinforced with paper tapes provides optimal cosmesis. The patient is returned to the recovery room with the arm in continuous passive motion to minimize the tendency to form adhesions in the humeroscapular motion interface (see figure 66).
The patient is taught passive mobilization of the shoulder to 140 degrees of elevation (see figures 67 and 68) and 40 degrees of external rotation (see figure 69) as well as stretching of the posterior capsule (see figures 70 and 71) and is discharged from the medical center when these goals are achieved. Active use of the shoulder with the arm at the side is instituted immediately. Sling immobilization is unnecessary. Strengthening of the deltoid and residual cuff muscles is started six weeks after surgery. An ideal exercise for optimizing the strength of active elevation is the progressive supine press (see figure 72). In this exercise small increments are used to train the remaining muscles to optimal advantage. Note that the scapular muscles are also put to work in these exercises (see figures 73 and 74). This program is easy for the patient to learn and to carry out alone.
Failed cuff surgery
In this condition the patient is dissatisfied with the result from a previous arthroscopic or open operation on the rotator cuff and presents for consideration of additional surgery.
Causes of failure
Rotator cuff repair may fail to yield a satisfactory result for many reasons including failure to obtain preoperative expectations of strength and comfort infection deltoid denervation deltoid detachment loss of the acromial lever arm adhesions in the humeroscapular motion interface persisting subacromial roughness denervation of the cuff failure of the cuff repair retear of abnormal tendon failure of grafts to "take failure of rehabilitation, and loss of superior stability. Effective treatment of these failures depends on the establishment of the proper diagnosis. Infection requires culture-specific antibiotics and irrigation and drainage if purulence is present. A prompt definitive approach may prevent joint surface destruction. Acute failure of the deltoid reattachment requires prompt repair before muscle retraction becomes fixed. Chronically painful and functionally limiting postoperative scarring often responds to gentle, frequent stretching at home. Shoulder manipulation in this situation is inadvisable because of the risk of cuff damage. However, in certain shoulders that are refractory to rehabilitation, substantial improvement in comfort and function can be achieved by an open lysis of adhesions and subacromial smoothing, followed by early assisted motion. Weakness of shoulder elevation often responds to gentle, progressive strengthening of the anterior deltoid and external rotators.
Persistent weakness requires evaluation for possible neurological injury or cuff failure. Denervation of the deltoid is diagnosed by selective electromyography of the anterior muscle fibers. In selected cases anterior deltoid denervation may be treated by anterior transfer of the origin of the middle deltoid with closure to the clavicular head of the pectoralis major although consistently good results from this procedure have not been documented. Denervation of the supraspinatus and infraspinatus or subscapularis is diagnosed by selective electromyography and is difficult to manage. Postoperative cuff failure is suggested by failure of the patient to regain strength of external rotation or elevation of the shoulder subacromial snapping and upward instability of the humeral head. In this situation arthrography may not be reliable; false-negative results from scarring or false-positive results from inconsequential leaks reduce the diagnostic accuracy. In our experience expert dynamic cuff ultrasonography provides the most specific data on cuff thickness and integrity. Repeat cuff exploration with smoothing or repair may be considered although the patient is warned that the tissue may be of insufficient quantity and quality for a durable re repair. Loss of superior stability can result when the coracoacromial arch has been sacrificed without reestablishing stability with a durable cuff repair. The deltoid becomes stretched so that the humeral head seems to be just below the skin. Patients who lose stability and deltoid function are some of the most unhappy we encounter after previous repair attempts.
The results of surgery for failure of previous cuff repairs are inferior to those of primary repair. DeOrio and Cofield (DeOrio and Cofield 1984) reviewed their experience with re repairs. At a minimum of two years' follow-up (average four years) 76 percent of patients had substantial diminution of pain; however 63 percent still had moderate or severe pain. Only seven patients gained more than 30 degrees of abduction and only four patients were felt to have a good result. The authors suggest that the main benefit of repeat cuff surgery is likely to be a reduction in discomfort.
Harryman et al (Harryman Mack 1991) however showed that if cuff integrity is durably established at revision surgery the results were comparable to those of primary repairs.
Arthrodesis
When a shoulder has been devastated by infection deltoid detachment or denervation intractable cuff failure or denervation and/or acromionectomy consideration is given to shoulder arthrodesis. Under these circumstances a glenohumeral arthrodesis provides a salvage option: by securing the humeral head to the scapula the scapular motors can be used to power the humerus through a very limited range of humerothoracic motion.
The best candidates for this procedure are those patients with
- permanent and severe weakness due to loss of cuff and deltoid function
- good bone stock
- a good understanding of the limitations and potential complications of a shoulder fusion
- intact scapular motors
- good motivation
- minimal complaints of pain and
- a functional contralateral shoulder.
To establish the limitations of shoulder fusions we studied twelve patients who had glenohumeral arthrodeses at least two years prior to the time of study. (Matsen Lippitt 1994) In these patients elevation in the plus 90 degrees (anterior sagittal) plane averaged 47 degrees. Elevation in the minus 90 degrees (posterior sagittal) plane averaged 22 degrees. External rotation averaged 9 degrees and internal rotation 46 degrees. These ranges of motion were similar to the scapulothoracic motion measured in normal subjects. Only one of the patients could reach his hair without bending his neck forward only five could reach their perineum six could reach the back pocket seven the opposite axilla and ten the side pocket.
We also studied normal in vivo shoulder kinematics to predict the functions which would be allowed by various positions of glenohumeral arthrodesis assuming that the scapulothoracic motion would remain unchanged. Using the normal scapulothoracic motions we were able to model the functional effects of fusion positions. We found that activities of daily living could be best performed if the joint was fused in 15 degrees of flexion 15 degrees of abduction and 45 degrees plane and 45 degrees of internal rotation (see figure 75). This low angle of elevation and relatively high degree of internal rotation facilitated reaching the face opposite axilla and perineum.
About cuff tear arthropathy
Rotator cuff tear arthropathy (or shoulder arthritis with a large rotator cuff tear) is a severe and complex form of shoulder arthritis in which the shoulder has lost not only the cartilage that normally covers its joint surface but also the tendons of the rotator cuff tear which help position and power the joint.
Normally the tendons of the rotator cuff (large arrows) allow smooth motion of the upper end of the arm bone (humerus) beneath the overlying bones and muscles.
When the rotator cuff is degenerated chronically torn or otherwise deficient the normally smooth upper surface of the upper end of the arm bone (humeral head) is unprotected from rubbing with the undersurface of the bone and ligaments above.
In cuff tear arthropathy the upper surface of the ball of the upper arm bone (humeral head) becomes roughened as it rubs against the overlying bone (the acromion). This condition results in shoulder pain weakness stiffness and grinding on movement.
Treatment options for cuff tear arthropathy include partial joint replacement with a cuff tear arthropathy (CTA) prosthesis. If severe instability of the joint complicates cuff tear arthropathy a reversed (reverse Delta) prosthesis may be indicated.
In this condition resisted isometric contraction of the cuff muscles is weak; acromiohumeral and often glenohumeral movements produce crepitance; radiographs demonstrate superior translation of the head of the humerus with respect to the acromion loss of the articular cartilage of the superior humeral head direct articulation of the head with the coracoacromial arch "femoralization" of the proximal humerus and "acetabularization" of the upper glenoid and coracoacromial arch (see figures 76-79).
The combination of glenohumeral joint surface destruction and massive cuff deficiency can be devastating. (Neer Craig 1983) Yet each patient has an individual combination of pain and functional losses. Patients with mild pain are managed with mild analgesics and gentle function-maintaining exercises.
When chronic cuff deficiency with upward displacement of the humeral head leads to repeated abrasive contact between the upper humerus and the coracoacromial arch and symptomatic destruction of the humeral articular cartilage reconstructive options are seriously limited. Shoulder arthrodesis is unattractive because these patients are often older and the condition may be bilateral. (Neer 1983) Constrained total shoulder arthroplasty is an option but the failure rate is very high. Secure cuff reconstruction with unconstrained total shoulder arthroplasty is usually impossible owing to massive cuff tissue deficiency. (Franklin Barrett 1988) Unconstrained arthroplasty without a secure cuff repair carries a high incidence of eccentric loading and "rocking horse" loosening of the component (see figure 80). (Franklin Barrett 1988 Matsen Lippitt 1994)
In a 1986 report to the ASES Brownlee and Cofield reported on 20 surgical procedures for cuff tear arthropathy. (Brownlee and Cofield 1986) These included Neer-type total shoulder arthroplasty total shoulder arthroplasty using a hooded glenoid and proximal humeral replacement without a glenoid. Extensive mobilization of tendons was attempted for repair. Pain relief was substantial in each group. Active abduction was best in the group with proximal humeral replacement. Three of the glenoid components loosened.
Arntz et al (Arntz Jackins 1993) reported our results in 19 patients 54 to 84 years of age who had disabling pain attributable to a massive tear of the rotator cuff accompanied by loss of the surface of the glenohumeral joint. These patients were not considered candidates for total shoulder replacement because of the massive deficiency in the cuff and the fixed upward displacement of the humeral head (see figures 76-79). A prerequisite for hemiarthroplasty was a functionally intact coracoacromial arch to provide superior secondary stability for the prosthesis. One important aspect of the operative technique was the selection of a sufficiently small prosthetic head volume so that excessive tightness of the posterior aspect of the capsule could be avoided (see Chapter 16 for discussion of "overstuffing"). Eighteen shoulders in sixteen patients were available for follow-up which ranged from twenty-five to 122 months. Pain decreased from marked or disabling in fourteen shoulders preoperatively to none or slight in ten and to pain only after unusual activity in four. Active forward elevation improved from an average of 66 degrees preoperatively to an average of 109 degrees postoperatively. One patient who had had an excellent result fell and sustained an acromial fracture so the functional result changed to poor. Three patients had persistent substantial pain in the shoulder that led to a revision. Neither infection nor prosthetic loosening developed in any shoulder.
In a separate report Arntz et al (Arntz Matsen III 1991) reviewed 23 shoulders in 23 patients with disabling pain associated with irreparable tears of the musculotendinous cuff. 12 shoulders with preserved passive motion normal deltoid function loss of glenohumeral joint surfaces and sculpturing of the coracoacromial arch received a reconstruction with a humeral hemiarthroplasty. In another 11 shoulders that failed to meet these prerequisites or that demanded heavy use after operation glenohumeral arthrodesis was selected. Comfort level and overall function were improved in both groups. Active forward elevation improved an average of 44 degrees in the hemiarthroplasty group and an average of 15 degrees in the arthrodesis group. These results coupled with the problems of glenoid loosening reported when total shoulder arthroplasty (see figure 80) is performed in the presence of cuff deficiency with upward head displacement suggest that humeral hemiarthroplasty is the preferred method for managing complex irreparable tears of the rotator cuff in which the articular surface is destroyed yet the deltoid muscle is functional (see figures 78 81 and 82). Shoulder arthrodesis is reserved for those patients who have both irreparable tears of the rotator cuff and irreparable deficiencies of the deltoid muscle or the younger patient with demands for substantial strength at low angles of flexion (see figure 83).
Authors' preferred method for cuff tear arthropathy
In the reconstruction for cuff tear arthropathy we attempt to make use of the "femoralization" of the proximal humerus (i.e. rounding so that the prominence of the tuberosities is lost) and the "acetabularization" of the gleno-coraco-acromial socket (i.e. erosion of the upper aspect of the glenoid and congruent concavity of the coracoacromial arch) (see figures 77-79). We have found that this adaptive ball and socket joint can be effectively and safely resurfaced using a humeral hemiarthroplasty (see figures 81 and 82). The goals of surgery are:
- assuring a smooth coracoacromial arch (usually already created by the process itself) avoiding acromioplasty and coracoacromial ligament section which would destroy the superior constraint of the humeral head;
- debriding useless fragments of cuff and bursa;
- anatomically resurfacing the destroyed humeral articular surface with a humeral endoprosthesis which will articulate with the coracoacromial arch and at all costs preserving the deltoid. We do not advocate cuff repair in this context nor the use of double cups or oversized humeral head prostheses. Instead the goal is to maintain the normal capsular laxity allowing internal rotation of the abducted arm to approximately 60 degrees.
Postoperatively the patient is started on continuous passive motion (see figure 84) and allowed activities as comfort permits.
127