Reverse Shoulder Replacement for arthritis and massive rotator cuff tears
Surgery with a reverse prosthesis can lessen shoulder pain and improve function in shoulders with failed surgery or combined arthritis, rotator cuff tears and instability
- Reverse Total Shoulder for Combined Shoulder Arthritis and Massive Rotator Cuff Tear and for Failed Conventional Total Shoulder Replacement
- Download this article in pdf format.
In this article
- Overview
- Reverse Total Shoulder Videos
- Symptoms
- Diagnosis
- Non-Surgical Treatment
- Reverse Shoulder Replacement Surgery
- Physical Therapy and Recovery
- Summary
Overview
The reverse total shoulder replacement arthroplasty enables experienced shoulder surgeons to treat patients with conditions that previously had no solution. These conditions include rotator cuff tear arthropathy, instability with anterosuperior escape, pseudoparalysis, and failures of surgery for arthritis and facture management.
Rotator cuff tear arthropathy (arthritis with a large cuff defect) is a devastating condition that seriously compromises the comfort and function of the shoulder. This condition is characterized by the irreparable loss of the rotator cuff tendons and destruction of the normal joint surface of the shoulder. Because these tissues cannot be restored, the shoulder is often weak painful and unstable. Using special techniques and a reversed total shoulder design (See Fig. 1 and 2 ), qualified surgeons can improve the stability of the shoulder and enable the deltoid muscle to power it, even in the absence of a normal rotator cuff.
By contrast, when the rotator cuff is intact, shoulder arthritis is often best treated by a total shoulder replacement. In certain milder cases of rotator cuff tear arthropathy without instability a special prosthesis with a CTA head may be indicated.
Failed conventional shoulder joint replacements and failed fracture surgery may also be treatable using a reverse total shoulder replacement.
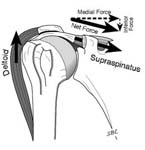
In the normal shoulder, the rotator cuff muscles, including the supraspinatus, help balance the ball of the arm bone (humeral head) in the socket against the upward pull of the deltoid muscle (See Fig. 3).
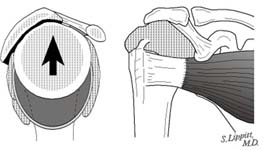
In rotator cuff tear arthropathy, the rotator cuff tendons that normally are interposed between the humeral head and the overlying coracoacromial arch become progressively thinned until the humeral head moves upwards and rubs against the bone of the arch (See Fig. 4).
In the early stages of rotator cuff tear arthropathy, the humeral head remains centered in the socket (glenoid) in spite of a large rotator cuff tear (See Fig. 5). In later stages of rotator cuff tear arthropathy, the humeral head migrates upwards but is stabilized by the overlying coracoacromial arch in spite of the lack of rotator cuff (See Fig. 6). In the severe stage of rotator cuff tear arthropathy, the humeral head is unstable, migrating upwards and forwards because it is no longer held in position by the coracoacromial arch. This condition often arises after previous procedures, such as an acromioplasty performed in the presence of a large cuff tear (See Fig. 7). In this situation the arm often cannot be raised from the side even though the deltoid muscle is working; this is called 'pseudoparalysis'.
After performing a clinical exam, a shoulder surgeon experienced with rotator cuff tear arthropathy can suggest what type of surgery is most likely to be helpful to the individual with the condition. Individuals are most likely to benefit from reverse shoulder replacement surger if they are well motivated and in good health.
Shoulders with active elevation of 90 degrees or more (indicating good deltoid tension and stability) may be treated with shoulder arthroplasty using a cuff tear arthropathy (CTA) prosthesis.
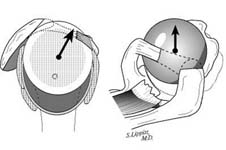
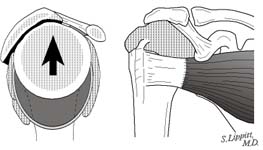
Shoulders with anterosuperior escape and pseudoparalysis (inability to actively raise the arm above 45 degrees) are considered for the reversed total shoulder prosthesis because other options may not provide sufficient stability for the humeral head (ball of the shoulder joint). The reversed total shoulder prosthesis is designed with a socket where the ball (head of the humerus) is normally located and a ball where the socket (glenoid) is usually located. This configuration adds stability so that the deltoid muscle can power the shoulder.
The goal of reverse total shoulder replacement is to restore some function to the joint destroyed by cuff tear arthropathy. Reverse total shoulder replacement restores function by providing stability and a fulcrum against which the deltoid muscle can help elevate the shoulder to a level where some basic shoulder functions can be performed.
Reverse total shoulder replacement is a highly technical procedure and is best performed by a surgical team who has experience with this surgery. Such a team can maximize the benefit and minimize the risks of surgery.
The two-hour reverse total shoulder replacement is performed under general anesthesia.
Use of the arm is started several weeks after the procedure. Extensive therapy is not needed with reverse shoulder surgery.
This procedure does not restore the ability of the shoulder to perform heavy work or sport.
Reverse Total Shoulder Image Gallery
Click an image below to enlarge and enter the gallery.
Reverse Total Shoulder Replacement Videos
In the two videos below, Dr. Frederick Matsen, UW Medical Center orthopedic surgeon, discusses a new and innovative shoulder replacement surgery featuring a reverse ball/socket technique that can lessen pain and improve function in shoulders with failed surgery or combined arthritis, rotator cuff tears and instability issues. Sheila Cape, one of Dr. Matsen's patients, discusses her previous unsuccessful surgical procedures to restore functionality to a shoulder with extensive rotator cuff damage before she came to the UW Medical Center where the Delta surgery was successfully performed. Discussion of research and rehabilitation along with surgery footage is also highlighted.
Reverse Shoulder Replacement, Part 1
Reverse Shoulder Replacement, Part 2
10 surgery questions for your surgeon before having surgery
Symptoms of rotator cuff tear arthropathy
Characteristics of rotator cuff tear arthropathy
Rotator cuff tear arthropathy (or shoulder arthritis with a large rotator cuff tear) is a severe and complex form of shoulder arthritis in which the shoulder has lost not only the cartilage that normally covers its joint surface, but also the tendons of the rotator cuff tear, which help position and power the joint (See Fig. 8).
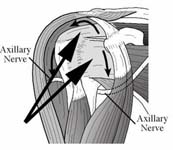
Normally the tendons of the rotator cuff (large arrows in Fig. 9) allow smooth motion of the upper end of the arm bone (humerus) beneath the overlying bones, ligaments, tendons, and muscles (See Fig. 9).
When the rotator cuff is degenerated chronically, torn, or otherwise deficient, the normally smooth upper surface of the upper end of the arm bone (humeral head) is unprotected from rubbing the undersurface of the bone and ligaments above (See the large arrow in Fig. 10).
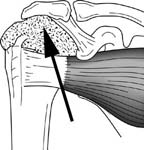
In cuff tear arthropathy, the upper surface of the ball of the upper arm bone (humeral head) becomes roughened as it rubs against the overlying bone (the acromion) (See the arrow in Fig. 11). This condition results in shoulder pain, weakness, stiffness, and grinding on movement.
Image Gallery of Rotator Cuff Arthropathy Symptoms
Similar conditions
Shoulder arthritis with a massive cuff defect must be distinguished from arthritis without substantial rotator cuff involvement, from isolated rotator cuff disease, from frozen shoulder, and from neck arthritis; each of which may produce somewhat similar symptoms. Arthritis usually gives rise to stiffness without weakness. Rotator cuff tears usually cause pain and weakness but stiffness is less common. Frozen shoulder is characterized by shoulder stiffness but the X-rays are usually normal. Neck arthritis may cause shoulder pain and weakness that is worse when the head is held in certain positions.
Incidence and risk factors
Rotator cuff tear arthropathy (or shoulder arthritis with a large rotator cuff tear) most commonly occurs in individuals over the age of 65 and is more common in women than men.
Diagnosis
Rotator cuff tear arthropathy (or shoulder arthritis with a large rotator cuff tear) is diagnosed by a history of progressive loss of shoulder function usually without an injury along with a physical examination showing weakness and grinding on movement and a typical appearance on X-ray. In these films the humeral head can be seen contacting the undersurface of the coracoacromial arch (indicated by the arrows in Fig. 12). The most important test for cuff tear arthropathy is the x-ray characteristically showing rounding off of the humeral head as it contacts with the undersurface of the coracoacromial arch. [See Fig. 13).
Rotator cuff tear arthropathy (arthritis of the shoulder associated with a massive cuff tear) is best diagnosed by an orthopedic surgeon with experience in shoulder disorders. Certain surgeons specialize in rotator cuff tear arthropathy (arthritis of the shoulder associated with a massive cuff tear).
Non-Surgical Treatment
Medications
Mild analgesic medications may relieve some of the symptoms of cuff tear arthropathy.
Exercises
If the symptoms of rotator cuff tear arthropathy (shoulder arthritis with a massive rotator cuff tear) are mild the condition may be treated with gentle motion exercises.
Surgical Treatment - Reverse Shoulder Replacement
Possible benefits of reverse shoulder
When exercises are not successful most cases of cuff tear arthropathy are considered possible candidates for shoulder joint replacement arthroplasty with a cuff tear arthropathy (CTA) head prosthesis that allows arthritic shoulders to regain some of their lost comfort and function. However, when the shoulder is no longer stabilized with the ball in the socket consideration can be given to a reversed (reverse Delta) prosthesis.
Joint replacement surgery can improve the mechanics of the shoulder but cannot make the joint as good as it was before the onset of rotator cuff tear arthropathy. The effectiveness of the procedure depends on the health and motivation of the individual, the condition of the shoulder, and the expertise of the surgeon. When performed by an experienced surgeon, shoulder replacement arthroplasty with reversed (reverse Delta) prosthesis can provide improved stability along with improved shoulder comfort and function.
The greatest improvements patients experience after reverse shoulder replacement are in the ability to sleep and to perform some of the simple activities of daily living. In that the tendons of the rotator cuff are not repairable in this condition, normal strength and function of the shoulder cannot be regained.
Types of surgery recommended
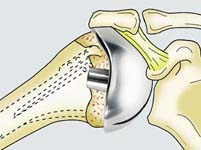
Three types of surgery can be helpful in the management of rotator cuff tear arthropathy (shoulder arthritis associated with massive rotator cuff defects). The surgical procedures can range from a simple smoothing of the roughened bone to a resurfacing of the humeral head with a smooth prosthesis, such as one with a rotator cuff tear arthropathy (CTA) head fixed to the shaft of the arm bone (humerus) (See Fig. 14). If the joint is unstable a reversed prosthesis such as the reverse Delta (See Fig. 15). may be needed.

Who should consider reverse shoulder?
Individuals with rotator cuff tear arthropathy complicated by shoulder instability should consider joint replacement surgery with a reversed prosthesis if:
- the cuff tear arthropathy complicated by instability is a major problem for the individual,
- the individual is sufficiently healthy to undergo the procedure,
- the individual understands and accepts the risks and alternatives,
- there is sufficient bone to permit the surgery,
- the surgeon is experienced in shoulder replacement surgery with a reversed (reverse Delta) prosthesis, and
- no other surgical options are preferable for the individual's shoulder.
Shoulder replacement surgery with a reversed prosthesis is most effective when the individual follows a simple exercise program after surgery and understand the limitations of the procedure. Thus, the individual motivation and cooperation are important elements of the partnership.
What happens without surgery?
The rate of progression of rotator cuff tear arthropathy (shoulder arthritis with a massive rotator cuff defect) is usually slow thus surgery is not urgent. However, serious instability with associated loss of function can motivate prompt surgical consideration.
Surgical options
Three types of surgery can be helpful in the management of rotator cuff tear arthropathy (shoulder arthritis associated with massive rotator cuff defects). The surgical procedures can range from a simple smoothing of the roughened bone to a resurfacing of the humeral head with a smooth prosthesis such as a cuff tear arthropathy (CTA) head fixed to the shaft of the arm bone (humerus). If the joint is unstable a reversed prosthesis may be needed.
Effectiveness of Surgery
In the hands of an experienced surgeon, shoulder arthroplasty with a reversed prosthesis can be helpful in restoring stability comfort and function to the shoulder of a well-motivated individual with cuff tear arthropathy complicated by instability. The greatest benefits are often the ability to sleep on the affected shoulder and the ability to perform simple activities of daily living. As long as the shoulder is cared for properly and subsequent injuries are avoided the benefit can last for years.
Urgency and Timing of Surgery
In that rotator cuff tear arthropathy progresses slowly, consideration of surgery is not urgent. Before surgery is undertaken the individual needs to be in optimal health, understand and accept the risks and alternatives of surgery, and understand the postoperative rehabilitation program. Only if there is concern about the possibility of infection in a swollen, warm, and red shoulder does urgent surgery demand consideration. If there is an infection, prosthesis would not be inserted, but rather, the shoulder would require surgical cleaning out and extensive postoperative antibiotics.
Shoulder replacement arthroplasty can be delayed until the time that is best for the individual's overall health and convenience. However, excessive delays can result in the loss of bone making the reconstruction more difficult for the surgeon and the individual.
Risks of Surgery
Shoulder replacement surgery for rotator cuff tear arthropathy using a reversed prosthesis carries significant risks that are important for the individual to consider. The risks of this surgery include but are not limited to the following:
- infection (which can be sufficiently serious to require revision surgery, including removal of the prosthesis)
- injury to nerves and blood vessels
- fracture
- stiffness or instability of the joint
- dislocation
- loosening of the prosthesis
- pain
- failure of tendon or muscle attachment
- the need for additional surgeries
Any of these problems may result in major loss of function to the arm. There are also risks of anesthesia and blood transfusion (although transfusions are not usually necessary). An experienced shoulder joint replacement team will use special techniques to minimize these risks but cannot totally eliminate them. After surgery there is a risk of fracture if excessive loads are applied to the arm. Thus, prevention of falls is very important.
Managing Surgical Risk
Some of the risks of shoulder replacement surgery with a reversed prosthesis can be effectively managed if they are promptly identified and treated. Infections may require a wash out in the operating room. Sometimes complete removal of the prosthesis is necessary. Blood vessel or nerve injury may require repair. Fracture may require surgical fixation. Stiffness or instability may require exercises or additional surgery. Loosening of the prosthesis may require surgical revision. If the individual has questions or concerns about the course after surgery the surgeon should be informed as soon as possible.
How to Prepare for Reverse Total Shoulder Surgery
Shoulder joint replacement surgery with a reversed prosthesis is considered for healthy and motivated individuals in whom cuff tear arthropathy is complicated by instability that interferes with the comfort and function of the shoulder.
Successful shoulder replacement depends on a partnership between the individual and the experienced shoulder surgeon. Individuals should optimize their health so that they will be in the best possible condition for this procedure. Smoking should be stopped a month before surgery and not resumed for at least three months afterwards. Any heart, lung, kidney, bladder, tooth, or gum problems should be managed before surgery. Any infection may be a reason to delay the operation. The shoulder surgeon needs to be aware of all health issues including allergies and the non-prescription and prescription medications being taken. Some of these may need to be modified or stopped. For instance, aspirin and anti-inflammatory medication may affect the way the blood clots. The area of the skin incision must be clean and free from sores and scratches.
Before surgery the individual should consider the limitations, alternatives, and risks of surgery. Individuals should also recognize that shoulder replacement with a reversed prosthesis cannot restore normal function to the severely damaged shoulder.
The individual needs to plan on carefully protecting the arm for three to six weeks after the procedure. Driving, shopping, and performing usual work or chores may be difficult after surgery. Plans for necessary assistance need to be made before surgery. For individuals who live alone or those without readily available help, arrangements for home help should be made well in advance.
Costs
The surgeon's office should provide a reasonable estimate of the surgeon's fee and the hospital fee.
Surgical team
Shoulder replacement arthroplasty with a reversed (reverse Delta) prosthesis for cuff tear arthropathy complicated by instability is a technically demanding procedure that should be performed by an experienced surgeon in a medical center experienced in performing similar shoulder joint replacements. Individuals should inquire as to the number of shoulder arthroplasty procedures that the surgeon performs each year and the number of these procedures performed in the medical center each year.
Finding an experienced surgeon
Because relatively few shoulder arthroplasties are performed in the United States each year it is unlikely that every community has an experienced shoulder arthroplasty surgeon who frequently performs arthroplasties for cuff tear.
Facilities
Shoulder replacement arthroplasty is usually performed in a major medical center that performs these procedures on a regular basis. These centers have surgical teams and facilities specially designed for this type of surgery. They also have nurses and therapists who are accustomed to assisting individuals in their recovery from shoulder replacement surgery.
Anesthetic
Shoulder joint replacement surgery is usually performed under a general anesthetic.
Length of reverse shoulder replacement surgery
The procedure usually takes approximately two hours, however, the preoperative preparation and the postoperative recovery may add several hours to this time. Individuals often spend two hours in the recovery room and two to four days in the hospital after surgery.
Pain and pain management
Recovery of comfort and function after humeral prosthetic arthroplasty with a cuff tear arthropathy head is progressive after the surgery. Often the benefits become apparent to the individual after two to six weeks.
This replacement procedure is a major surgical procedure that involves cutting of skin, tendon, and bone and removal of scar tissue, as well as resuturing of tendon back to bone. The pain from this surgery is managed by the anesthetic and by pain medications. Immediately after surgery, strong medications (such as morphine or Demerol) may be given by injection and by mouth as needed. Within a day or so, oral pain medications (such as hydrocodone or Tylenol with codeine) are usually sufficient. On the other hand, some individuals need surprisingly little pain medication after this procedure. In older individuals it is often safer to use relatively less pain medication.
Use of medications
Initially after surgery pain medication can administered by mouth, in the vein (intravenously), or in the muscle (intramuscularly). Sometimes patient controlled analgesia (PCA) is used to allow the individual to administer the medication as it is needed. Hydrocodone or Tylenol with codeine are taken by mouth. Intravenous pain medications are usually needed only for the first day or two after the procedure. Oral pain medications are usually needed only for the first two weeks after the procedure. Some individuals need surprisingly little pain medication after this procedure. In older individuals it is often safer to use relatively less pain medication.
Effectiveness of medications
Pain medications can be very powerful and effective. Their proper use lies in the balancing of their pain relieving effect and their other less desirable effects (such as slowed breathing, sleepiness, nausea, constipation, or difficulty urinating). Good pain control is an important part of the postoperative management.
Important side effects of pain medications
Pain medications can cause drowsiness, slowness of breathing, difficulties in emptying the bladder and bowel, nausea, vomiting, and allergic reactions. Individuals who have taken substantial narcotic medications in the recent past may find that usual doses of pain medication are less effective. For some individuals, balancing the benefit and the side effects of pain medication is challenging. Individuals should notify their surgeon if they have had previous difficulties with pain medication or pain control.
Hospital stay
After surgery the individual spends an hour or so in the recovery room. A drainage tube is usually used to remove excess fluid from the surgical area. The drain is usually removed on the second day after surgery. Bandages cover the incision. They are usually changed the second day after surgery. Individuals are discharged as soon as the incision is dry the shoulder is comfortable with oral pain medications the individual can care for the shoulder and the home support systems for the individual are in place. Discharge is usually on the third or fourth day after surgery.
Recovery and rehabilitation in the hospital
Early, protected, and restricted motion after shoulder replacement with a reversed (reverse Delta) prosthesis helps achieve the best possible shoulder function. The surgeon will provide detailed information on the optimal program after the particular surgical procedure.
During the hospitalization the individual learns a simple rehabilitation program that will be used at home after discharge. The arm is kept in a sling for several weeks after surgery to allow for early healing.
Hospital discharge
At the time of discharge the individual should be relatively comfortable on oral medications, should have a dry incision, should understand their exercises, and should feel comfortable with the plans for managing the shoulder. For the first month or so after this procedure the operated arm may be less useful than it was immediately beforehand.
The specific limitations can be specified only by the surgeon who performed the procedure. It is important that the reconstructed shoulder not be challenged until it has had a chance to heal. Usually the individual is asked to lift nothing heavier than a cup of coffee for six weeks after the surgery.
Management of these limitations requires advance planning to accomplish the activities of daily living during the period of recovery.
Physical Therapy and Recovery
Convalescent assistance
Individuals usually require some assistance with self-care activities of daily living shopping and driving for at least six weeks after surgery. They usually go directly home after this surgery especially if there are people at home who can provide the necessary assistance or if such assistance can be arranged through an agency. In the absence of home support a convalescent facility may provide a safe environment for recovery.
Recovery of comfort and function after shoulder arthroplasty continues for many months after the procedure. Improvement in some activities may be evident as early as six weeks. With persistent effort individuals can make progress for as long as a year after surgery.
Physical therapy
Limited use after total shoulder replacement with a reversed prosthesis is critical for protection during the early phases of healing. In most cases we keep the arm in a sling for six weeks after the procedure to allow for healing of the soft tissues. Most individuals find the recovery of comfort and function can be accomplished without formal physical therapy.
Rehabilitation options
It is often most effective for the individual to carry out her or his own rehabilitation at home. Often no physical therapy is recommended.
Can rehabilitation be done at home?
In general the rehabilitation is best performed by the individual at home. Occasional visits to the surgeon or therapist may be useful to check the progress and to review the program.
Usual response to physical therapy
Individuals are almost always satisfied with the increases in comfort and function that are achieved with the rehabilitation program. If the exercises are uncomfortable difficult or painful the individual should contact the surgeon promptly.
Risks
The rehabilitation program is safe with little risk.
Duration of rehabilitation
Once the rehabilitation goals are achieved the exercise program can be cut back to a minimal level.
Returning to ordinary daily activities
In general individuals are able to perform gentle activities of daily living with the operated arm at the side starting four weeks after surgery. Walking with the arm protected is strongly encouraged. Driving should wait until the individual can perform the necessary functions comfortably and confidently. This may take up to six weeks if the surgery has been performed on the right shoulder because of the increased demands on the right shoulder for shifting gears.
With the consent of their surgeon individuals may be able to return to certain activities at six months after surgery. It is important to remember that shoulder arthroplasty with a reversed prosthesis does not restore the function of the degenerated rotator cuff tendons so that the shoulder will never totally regain full comfort strength range of motion or function. Stressful activities and activities with the arm in extreme positions may never be possible after this procedure.
Long-term patient limitations
Individuals should avoid activities that involve major impact (chopping wood contact sports activities with major risk of falls) or heavy loads (lifting of heavy weights heavy resistance exercises) after this surgery. In this way the risk of re-injury is minimized.
Costs of physical therapy
The surgeon and therapist should provide the information on the usual cost of the rehabilitation program. The program is quite cost-effective because it is based heavily on home exercises.
Summary of reverse shoulder replacement for rotator cuff tear arthropathy
Rotator cuff tear arthropathy (arthritis with a massive cuff defect) with shoulder instability is a devastating condition that seriously compromises the comfort and function of the shoulder. This condition is characterized by the permanent loss of the rotator cuff tendons and the normal surface of the shoulder joint. These tissues cannot be restored to their normal condition and the lost comfort and function of the shoulder cannot be totally regained.
However in the hands of an experienced surgeon and in a well-motivated individual shoulder replacement surgery with a reversed prosthesis along with careful post-surgical rehabilitation can help restore substantial comfort and function to shoulders damaged by cuff tear arthropathy and instability.
Pre-planning and persistent rehabilitation efforts will help assure the best possible result for the individual with rotator cuff tear arthropathy.
Follow Dr. Matsen's Shoulder Arthritis blog on which we try to provide the best and most current information on shoulder arthritis.
Contact
If you have questions regarding this article, feel free to email Frederick A. Matsen III M.D. at matsen@uw.edu.