Surgical options for early arthritis in young persons and athletes: the role of meniscus transplants, microfracture, Osteoarticular Transplants (OATs), Autologous Chondrocyte Implantation (ACI) and osteotomy
Edited By: Sports Medicine Team Last updated: Thursday, December 31, 2009 | |||||||||
| |||||||||
|
Patients who undergo a cartilage reconstruction require several months of rehabilitation to protect the repair and optimize regeneration of new cartilage. Normally a person can return to sedentary work after about 4- to 12-weeks. Depending on the procedure(s) performed, walking without the need for assistive devices occurs between 6-weeks and 12-weeks. The return to limited sporting endeavors, usually takes 6 to 9 months, and cutting athletics are usually not advised before 9- to 12-months after the surgery. Despite the difficulties in treating these lesions, good or excellent results can be expected in about 85% to 90% of persons, and a return to athletic activity is not uncommon.
Symptoms & Diagnosis
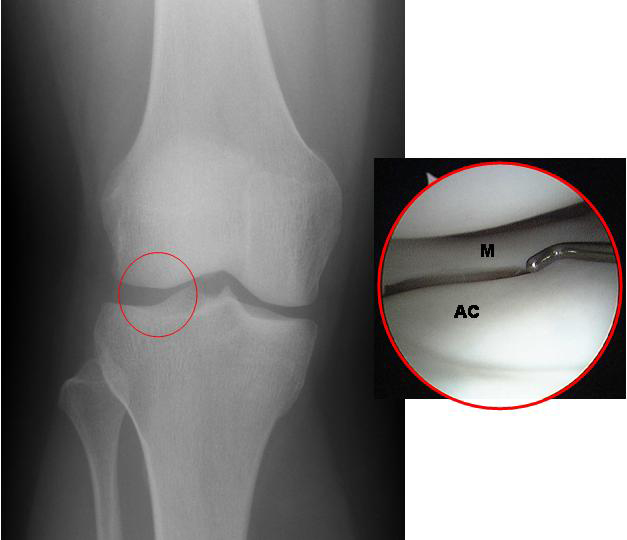
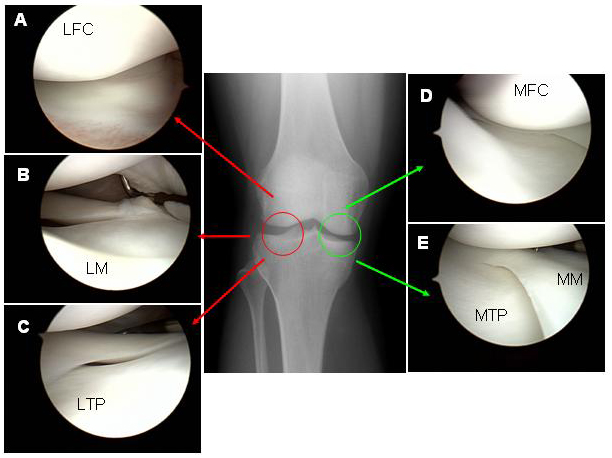
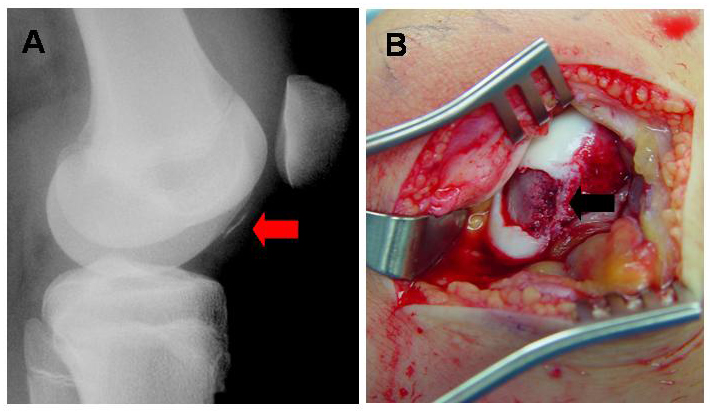
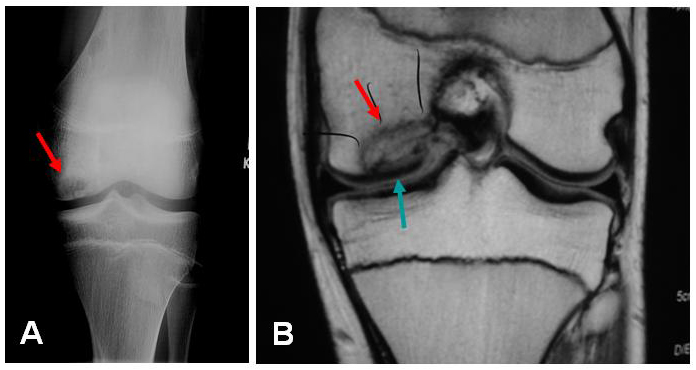
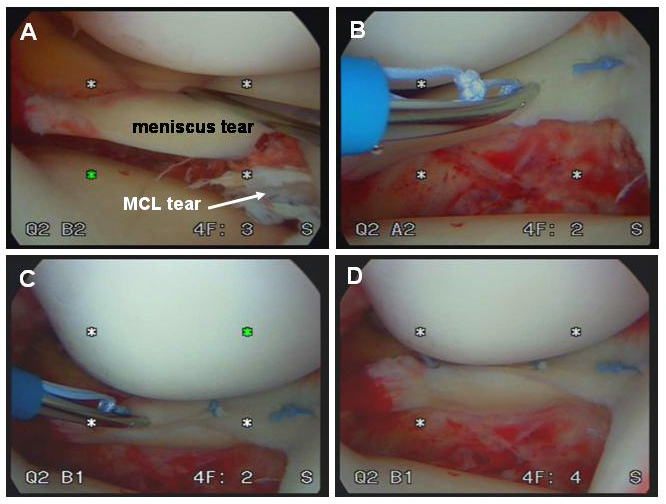
Characteristics of arthritis, osteochondral defects (ocd lesions), meniscus transplantation and cartilage loss in the knee. The loss of the articular cartilage in the knee is called arthritis by definition. The most common complaint is pain. This initially manifests as pain with certain activities or long days, but can progress to pain even at rest or prevent comfortable sleep. Frequently, patients will complain of swelling or have a “full” feeling after activities. If fragments of torn cartilage or the meniscus become trapped in the joint, a patient will experience sudden, sharp pains or locking of the joint. If the arthritis has been present for a long time, changes in the alignment of the joint (e.g. “bow-legs” or “knock-knees”) may begin to develop. The changes or pain may develop gradually over time, or can be the result of a traumatic injury, such as a fall or athletic injury. Types Cartilage is the term used to describe two different structures in the knee: the articular cartilage (a smooth gliding surface covering the end of the bone—analogous to the Teflon™ in a non-stick frying pan) and meniscal cartilages (C-shaped “bumpers” between the bone ends that help to make the bones conform and absorb shock). Either or both of these “cartilages” can be damaged, and frequently when one is damaged the other is injured as a result. (Figure 1) In traumatic injuries to the articular cartilages, the cartilage may shear off the end of the bone, sometimes taking a bony fragment with it. (Figure 5) If diagnosed early, these “osteochondralcartilage defects” can frequently be repaired surgically and will heal. These injuries are very different from OCD lesions described below, as the remaining bone beneath the cartilage is healthy. These cartilage lesions can be small (focal) or large (global). With osteochondral defects, the treatment plan is to repair the defect if possible, or replace the small region of affected cartilage with a substitute. Occasionally, the bone beneath a region of cartilage may lose its blood supply and die. (This can occur even without a traumatic injury to the knee). Because the articular cartilage receives its nourishment predominantly from the underlying bone, the cartilage may then also die and can fragment. These lesions are called “osteochondritis dissecans” (OCD) lesions. (Figure 6) To repair these lesions, the cartilage AND underlying bone must be considered. OCD lesions can be small (focal) or large (global). A similar condition is “avascular necrosis” (AVN). For these conditions, the treatment plan revolves around restoring a normal joint contour and replacing the damaged or dead cartilage and bone with a substitute. “Degenerative” lesions, are those that occur gradually. While they occasionally result from traumatic injury, they are more commonly related to subtle problems with joint alignment or long-term overuse of the joint. Most degenerative cartilage lesions are global lesions that involve a large portion of the weight-bearing region of the joint. When these lesions are large, the treatment may involve re-aligning the joint to shift stress away from the damaged cartilage, which slows the progression of the arthritis and decreases pain. Meniscal injuries occur commonly. When a small tear in the meniscus is present, it can usually be trimmed away (debrided). (Figure 7) However, if a large portion of the meniscus is, or has been, removed, the joint will eventually develop degenerative arthritis. In a young person or athlete in which most of the meniscus is removed, it is best to replace the meniscal tissue with a donor substitute (allograft). The timing of these meniscus transplants can be difficult, as the joint can feel healthy even without the meniscus for a time, but will become painful or swell as arthritis begins to develop. Ideally, the meniscus should be transplanted just as the joint is starting to become painful, but before any significant arthritis develops. Similar conditions Cartilage-restoration procedures (debridement, microfracture, OATs, ACI) are rarely indicated in a joint that suffers from moderate or severe degenerative osteoarthritis. Most persons with global arthritis or severe breakdown of the cartilage have developed changes in the joint that cannot be addressed by the restoration of small regions of cartilage. When both sides of the joint are involved (e.g. the “top” and “bottom” of the knee), the lesions are termed “bipolar.” The results of restoration procedures in these cases are less favorable, so the procedure is rarely performed. Small tears of the meniscus can be trimmed (debrided). (Figure 7) As long as the removed portion is relatively small, the improvement in symptoms is remarkable and the long-term drawbacks are minimal. Some larger meniscus tears are repairable.(Figure 8) If at all possible, meniscus repair is preferable to removal, particularly in younger patients. When the damage to the meniscus is extensive or irreparable, a person may wish to consider meniscal transplantation. (Figure 9) Arthritic conditions due to autoimmune or metabolic diseases, such as rheumatoid arthritis, lupus, or gout generally do not respond to cartilage restoration procedures. Tears of the ligaments (ACL, PCL, LCL, MCL) are also common and may cause a sense of “locking” or “instability” of the joint. While these can occur alongside cartilage injuries, their treatment is totally different. Incidence and risk factors Diagnosis The diagnosis of cartilage defects (osteochondral injuries, OCD lesions, AVN, etc.) and mensical lesions can be made in several ways. 1. Clinical exam: a skilled examiner can usually examine (relatively painlessly) the knee joint and discern which structures appear to be injured. 2. X-rays may identify a region of dead bone, abnormal contours in the joint surface, a displaced bone fragment (with cartilage attached), or abnormal alignments of the joint. 3. An MRI with an MRI arthrogram (MRI after an injection of contrast dye into the joint) will reveal:
MRI’s are extremely valuable in planning the appropriate reconstructive procedures. |
|
Treatments
Who should consider microfracture, meniscal transplantation, osteoarticular allograft/autograft transplants (oats), autologous chondrocyte implantation (aci) and osteotomy for arthritis in the athlete.? WHO SHOULD CONSIDER SURGERY FOR KNEE ARTICULAR CARTILAGE DEFECTS OR A DEFICIENT MENISCUS? Surgery should be considered as an option for a cartilage defect IMMEDIATELY when:
Surgery should be considered as an option for a chronic focal cartilage lesion if:
In addition, the following criteria must be met:
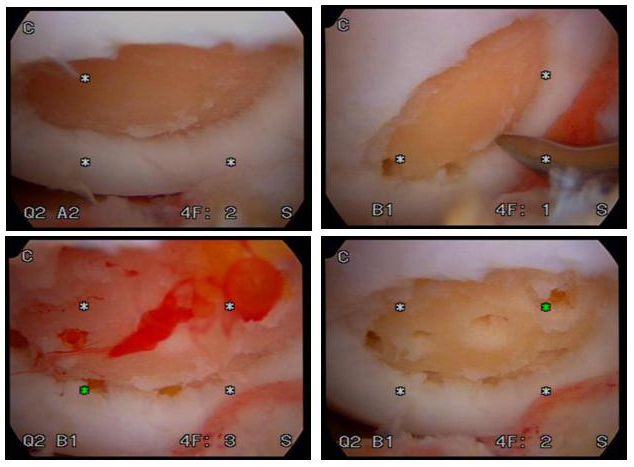
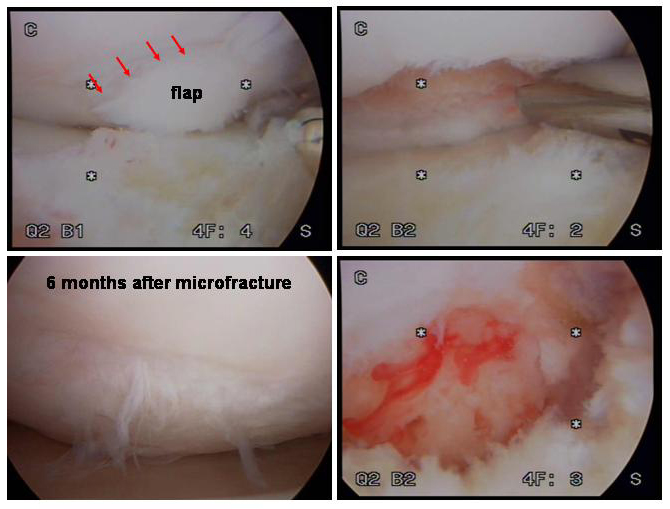
What happens without surgery? Unlike bone, articular cartilage does not “regrow”. For this reason, few lesions are capable of healing without treatment. One exception is osteochondritis dissecans (OCD). In this instance some persons (particularly the young) have some ability to heal these lesions without surgery provided the lesion does not “collapse” before the bone repairs itself. Early in their course, such lesions will cause discomfort, pain, swelling, and occasionally mechanical catching or grinding in the joint. This will prevent a person from enjoying her activities or will interfere with the normal functions of daily life. Most other cartilage injuries (osteochondral defects, avascular necrosis (AVN), traumatic cartilage injuries) and severe meniscal injuries will not heal. These lesions eventually affect the smoothness and structural integrity of the joints weight-bearing surface. Eventually, an untreated lesion may lead to premature global deterioration of the joint, severe pain, deformity, and disability. Surgical options Several options are available to the patient and the surgeon, depending on the nature of the lesion, the causes of the injury, and the age and activity level of the patient. Each procedure has an “ideal” indication, but the procedures can be used in conjunction to achieve the maximal benefit. It is essential that the surgeon be familiar with the patient, the problem, and all the treatment options in order to achieve the optimal result. MICROFRACTURE: Microfracture is a technique that was developed to “cover” small- to medium-sized bare regions of bone where the cartilage has been damaged but the bone beneath it is healthy. The concept is to use the arthroscope to prepare the healthy cartilage surrounding the bare spot and to create tiny vascular channels which run from the underlying bone’s blood supply to the defect. These vascular channels allow blood and the body’s reparative cells to enter the defect and create a fibrous scar (much like the way skin heals after a cut). Over time, the reparative scar matures and resembles articular cartilage. The mechanical properties of this reparative tissue do not equal that of native articular cartilage, but studies have shown that the majority of patients feel their pain is decreased and their function is improved after this procedure. In most cases, this procedure can be performed as an outpatient, but it requires 6 to 12 weeks of rehabilitation. The ultimate maturation of this tissue can take 4 to 6 months. (See Figure 10a, Figure 10b, Video 1, Video 2) Optimal indication: Patients of any age with small- to medium-sized lesions surrounded by normal cartilage. Microfracture can frequently act as a temporizing measure to allow the athlete a faster return-to-play than OATs or ACI procedures. Results: Long-term studies have demonstrated that even at up to 7 years follow-up, about 67% to 75% of patients have durable success with microfracture. OSTEO-ARTICULAR TRANSPLANTS OR OATs: Another technique which has been developed to treat small- to large-sized defects in articular cartilage is osteoarticular grafts or osteoarticular autograft transplants (OATs). The potential advantage of these techniques over microfracture is that they replace the injured articular cartilage with new articular-cartilage “plugs” which are taken from another region of the knee (autograft) or from a donated knee (allograft). When an autograft is used, the size of defect that can be filled is limited by the number of plugs that can be taken from another region of the knee without causing symptoms (2 to 4cm2 maximum). For very large lesions of the femur or patella, massive plugs can be taken from a donor knee and used to restore normal mechanics to the knee. While some OATs procedures can be done through minimal incisions with the use of an arthroscope, many OATs or donor graft procedures require an incision into the knee, and therefore a 1-to2-day hospital stay is required. Weight bearing is limited for a short time post-operatively and a home-based rehabilitation period is required. (see Figure 11a, Figure 11b) Optimal Indication: Patients aged 15 to 55 with small- to medium-sized lesions surrounded by normal cartilage. Normal or nearly normal cartilage on the adjacent joint surface. Results: Studies over the long term have demonstrated excellent results in 86 to 90 percent of cases for selected lesions. AUTOLOGOUS CHONDROCYTE IMPLANTATION: Autologous chondrocyte Implantation is a relatively new technique that takes advantage of the latest developments in biomedical engineering and orthopedic science. The concept behind ACI is to “harvest” a small sample of healthy cartilage cells from the injured knee and to “grow” them. In actuality, the cells are cultured in such a way that they multiply into a population of “chondrocytes” (or cartilage “precursor cells”). The grown chondrocytes are then introduced back into the defect in the knee, where they regenerate into mature cartilage-like tissue. The advantages of ACI include:
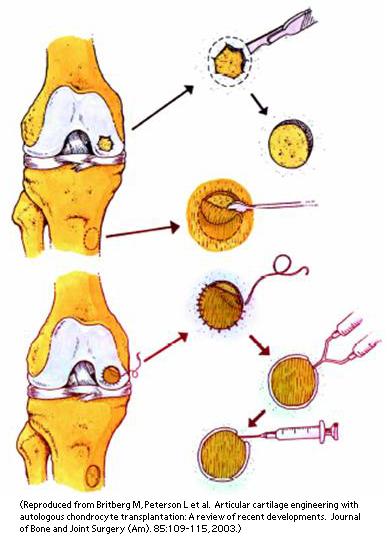
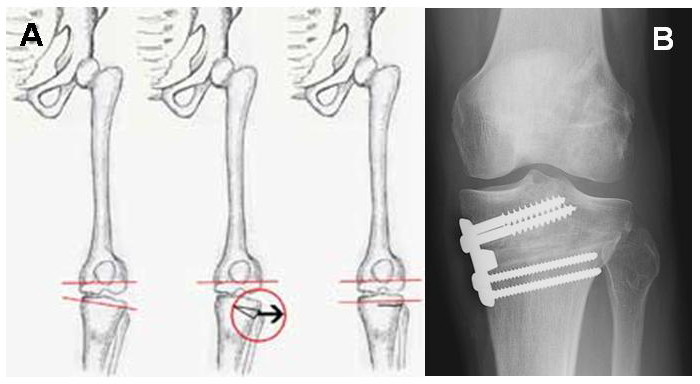
One disadvantage of ACI is that the architecture of the “grown” tissue is not normal, and therefore its biomechanical properties are different. Because it takes time to grow the precursor chondrocytes, ACI requires two separate surgical procedures. The initial procedure is completed through the arthroscope and includes an evaluation and harvest of a very small amount of articular-cartilage tissue (about the size of 5 or 6 grains of rice). Depending on the alignment of the knee, other surgical procedures may need to be performed at the initial surgery to maximize the benefit of the ACI procedure. The second procedure requires an open surgery of the knee, in which a small flap of tissue called “periosteum” is sewn to the perimeter of the defect (like putting a manhole cover over a hole in the pavement). The grown chondrocytes are then implanted beneath this cover. The first procedure is usually performed on an outpatient basis. The second procedure requires an open-knee incision, and usually requires a 1-to-2-day hospital stay. The patient usually must limit weight bearing for a short time, and a home-based rehabilitation period is required. (See Figure 12) Optimal indications: Patients between 15 and 55 years with medium-to-large, full-thickness cartilage loss or osteochondritis dissecans, who have normal or nearly normal cartilage on the adjacent joint surface, healthy underlying bone, and a normal joint contour. Results: Depending on the nature of the cartilage lesions, studies have shown good to excellent results 75 to 90 percent of persons. Recent studies have shown that in the short term, the cellular nature of tissue created by ACI may not be significantly different from that produced during microfracture. OSTEOTOMIES AND REALIGNMENT: An osteotomy is a procedure designed to re-align joint surfaces to shift the body weight away from damaged regions of the joint to the surfaces that are in better condition. A normal part of joint degeneration involves wear of the articular-cartilage surface, followed by “narrowing” of the joint space. This causes the limb to change its alignment (that is, patients become “knock-kneed” or “bow-legged”), which further places stress on the injured cartilage and causes even more severe injury. An osteotomy is a procedure in which the bone is cut, re-aligned, and re-fixed in a position that decreases the stress on injured cartilage. These procedures are frequently done in conjunction with cartilage-salvage (microfracture) or cartilage-restoration (OATs, ACI) procedures to help protect the repaired joint surface. (See Figure 13) Optimal indications: Patients between 15 and 60 years of age who engage in “high-demand” or “high-impact” activities that would not be tolerated by prosthetic replacements. Also patients who are candidates for cartilage salvage or cartilage reconstruction but have significant knee-alignment problems. Results: In the ideal patient population, successful results range between 80 and 93 percent. The durability of these results is variable, and it is generally accepted that patients can expect reliable symptomatic relief for 6 to 10 years. MENISCAL TRANSPLANTATION: Meniscal transplantation is done to replace a completely degenerated or destroyed meniscus. Transplants can be done for both the medial (inside) or lateral (outside) meniscal cartilages. The meniscus is replaced with a size-matched donated (allograft) meniscus cartilage that retains its normal bony attachment. When the meniscus is inserted, the bone is “grafted” into the patient; it will heal like a fracture would. The edges of the meniscus are sewn to the edge of the joint so that they will heal with the normal soft-tissue attachments as well. Once the allograft meniscus is healed, it assumes the functions of meniscal tissue and may prevent premature deterioration of the joint. (See Figure 9, Video 3) Optimal indications: In general, meniscus transplantation is performed in younger patients who have had severe meniscal injuries. It is ideal to replace the meniscus when the patient has symptoms but HAS NOT YET DEVELOPED significant secondary arthritic changes to the joint. Recent studies have shown some benefit using meniscal transplants to alleviate symptoms in knees in which arthritis HAS developed, but the long-term efficacy of this procedure is unknown. Results: The studies on meniscal transplantation are difficult to interpret, as many patients in these studies also undergo other procedures along with the transplant (ACL reconstruction, osteotomy, etc.). In general, 75 to 89 percent good results are obtained at short- and medium-term follow-up. Return to low-impact athletic is possible in the majority of persons. Most studies have demonstrated that between 5 and 14 years after the procedure, the transplanted meniscus can deteriorate and symptoms recur. JOINT ARTHROPLASTY: The techniques of joint replacement or arthroplasty have undergone a remarkable evolution over the past 30 years. All forms of arthroplasty involve the same concept: the removal of severely diseased or arthritic cartilage and bone and the reconstruction of the joint with synthetic fitted components. Because the new joint is man-made (it is usually metallic and plastic), it may wear out. For this reason, joint replacement is a last-resort procedure to relieve joint pain, malalignment, and cartilage loss in individuals who have moderate or low demands on their knees. There are three separate joints or “compartments” in the knee, and each can be replaced. When only a portion of the joint surface is affected, partial replacements are possible. “Unicompartmental” joint prostheses have been created to reconstruct only the medial (inside) or lateral (outside) bearing surfaces of the joint, and it is also possible to replace only the patellofemoral surface (between the kneecap and femur). Optimal indications: Patients older than 55 with severe osteoarthritis or joint collapse who engage in moderate- or low-demand activities. Results: The results of knee arthroplasty have been widely studied. Excellent or outstanding results can be expected in the vast majority of appropriately selected patients. The results of modern single-compartment (unicondylar and patellofemoral) procedures are currently being studied, but show promise. Effectiveness In the hands of an experienced surgeon familiar with all the available reconstructive options, cartilage restoration is usually very effective at eliminating or markedly decreasing pain, restoring function to the joint, and allowing a return to activity in the motivated patient. Depending on the procedure, the surgeon may discourage a return to high-impact (cutting, jumping, running) activities to prolong the viability of the reconstruction. The benefits of the above procedures may not be permanent, but in general their aim is to slow the progression of joint deterioration and preserve an active lifestyle for as long as possible. Urgency Surgical procedures are rarely urgent unless the lesion was caused by trauma and discovered immediately. If this is the case, it is frequently possible to repair rather than restore the injured cartilage. Saving the native cartilage is always the best option if it can be induced to heal. Once the lesion has become “chronic” or has been without a blood supply for an extended time, the surgical reconstruction is not an emergency. However, in general the restoration of smaller lesions produces better results than large ones. In the symptomatic patient, it is best to address a significant cartilage defect or meniscal injury before it leads to further deterioration of the joint. Before surgery is undertaken, the patient needs to: be in optimal health
Risks The risks of cartilage restoration procedures (microfracture, osteotomies, OATs, ACI, and mensical transplants) include but are not limited to the following:
The experienced and cautious surgical team uses special techniques to minimize all the above risks. Although adverse events following cartilage-restoration surgery are rare, they can occur and are not completely eliminated. Managing risk Many of the risks of surgery can be effectively managed if they are promptly identified and treated:
If a patient has questions or concerns about the “normal” course after surgery, the surgeon should be informed as soon as possible so that they can explain the expected course and outcome. Preparation Surgical cartilage restoration is considered for healthy and motivated individuals in whom pain and mechanical symptoms interfere with normal function and activity. Successful surgery depends on a partnership between the patient and an experienced knee surgeon. When possible, patients should optimize their health to prepare for surgery. Smoking should be stopped prior to surgery and avoided altogether for at least three to six months following surgery. Any heart, lung, kidney, bladder, tooth, or gum problems and concomitant injuries to the skin or extremity should be managed before the surgery. Any active infections will delay elective surgery to optimize the benefit and reduce the risk of joint infection. The surgeon should be made aware of any health issues, including allergies and non-prescription and prescription medications being taken. Some medications will need to be held or stopped prior to surgery. For instance, aspirin and anti-inflammatory medications (Advil®, Motrin®, Aleve®, and other NSAIDs) should be discontinued as they will affect intra-operative and postoperative bleeding. (Discuss this with the doctor who prescribed the medications.) Before surgery, patients should consider the limitations, alternatives, and risks to surgery. Patients must recognize that the procedure is a process and not an event: the benefit of the surgery depends largely on the patient’s willingness to participate inrehabilitation after surgery. Patients must plan on being less active and functional for 12 to 16 weeks after the surgery. Driving, shopping, lifting, walking, jogging, and running will be difficult or impossible if the surgery involves the weight-bearing joints. Plans for the necessary assistance need to be made before surgery. For individuals who live alone or those without readily-available help, arrangements for home help should be made early. If the surgery involves the knee or ankle, patients will be able to walk with support devices immediately after surgery, but they will be unable to bear weight on the operated leg for up to six weeks. Jogging is generally discouraged and is rarely resumed before 24 weeks. It takes 9 to 12 months for a full recovery. Costs The surgeon’s office should provide a reasonable estimate of:
Surgical team Cartilage restoration procedures (microfracture, OATs, ACI, meniscal transplantation, and osteotomies) are technically demanding procedures that must be performed by an experienced, specially trained orthopedic surgeon and skilled surgical team in a medical center accustomed to performing complex knee, shoulder, elbow and ankle procedures on a weekly basis. The surgical team of an orthopedic surgeon and certified physician assistant (PA-C) can dramatically improve the quality of care received by the patient. The interdependent physician-PA team ensures continuity of patient healthcare, commitment to personalized treatment, and makes certain patients will have greater access to care. The goal of this team is to magnify the efficiency and safety in the operating room and clinic, and to make certain the patient in receiving superior and quality care. Patients should ask about the specific training and experience the surgeon and surgical team has undergone to perform such procedures (i.e. a fellowship-trained, sports medicine specialist familiar with arthroscopic techniques and equipment). Finding an experienced surgeon While surgeons who are capable of performing simple arthroscopic procedures are relatively easy to find, complex cartilage replacement surgeries in the knee demand a degree of highly-specialized training. Many capable surgeons will have completed a fellowship (additional year or two of training) specifically in arthroscopic techniques, knee surgery, shoulder surgery, and sports medicine. A qualified sports-medicine surgeon should be comfortable with both open and arthroscopic techniques and tailor the appropriate treatment to injury. Fellowship-trained surgeons may be located through university schools of medicine, county medical societies, or state orthopedic societies. Other resources include professional societies such as the American Orthopedic Society for Sports Medicine (AOSSM) or the Arthroscopy Association of North America (AANA), and the American Academy of Orthopedic Surgeons (AAOS). Facilities Cartilage restoration is usually performed in a qualified ambulatory surgical center or major medical center that performs such procedures on a regular basis. These centers have surgical teams, facilities, and equipment specially designed for this type of surgery. Patients will usually require an overnight stay, and these centers have nurses and therapists trained to assist patients in their recovery from these procedures. Technical details Cartilage-restoration procedures are extremely complex; each step plays a critical role in the outcome. The procedures can be performed in the elbow, shoulder, hip, knee, and ankle. For the purposes of this explanation, procedures on the knee (the most commonly involved joint) will be discussed here. After the patient is comfortably positioned on the operating table and anesthetic has been administered, the knee is washed and draped. The surgeon begins by examining the knee while the patient is asleep; during this time the knee muscles are relaxed so the surgeon can assess the relative stability of the joint, the range of motion, and feel for any abnormal grinding or catching of the joint. Next, two or three very small (1cm) incisions, or “portals” are made, at the front of the knee. Through these small portals, hollow instruments called “canulas” are placed that irrigate the inside of the knee joint with sterile saline and “inflate” the joint with clear fluid. The canulas allow the placement of an arthroscopic camera and specially designed instruments within the knee joint. The surgeon maneuvers the camera around the joint while he or she watches a video monitor of what the camera “sees”. A highly-skilled surgeon can evaluate all of the important structures within the joint, test their stability and integrity, and look for signs of ligament injuries, cartilage wear (or arthritis), and bony injuries that can be caused by or lead to knee instability or mechanical grinding. (Video 1) Most often, the surgeon will take photographs of the interior of the joint to help explain to the patient what was found, and how it was corrected. This portion of the surgery is called a “diagnostic arthroscopy” and, in conjunction with a pre-surgical MRI, is absolutely necessary to assure the success of any surgical procedure for knee instability or cartilage deterioration. Once the surgeon understands the nature of the cartilage problem, he or she will choose the best possible surgical approach to treat it. Brief descriptions of the different procedures follow. Microfracture A microfacture technique is employed to create a scar tissue “cap” over a region of diseased cartilage. The concept takes advantage of the body’s own healing potential. A lesion in the cartilage is prepared so that the “shoulder” or edge of the lesion is surrounded by healthy cartilage. Then, the base of the lesion is stripped of all remnants of unhealthy cartilage debris, to a bare bone end. Next, specially-designed instruments, called “microfracture picks” are used to create small holes/channels in the base of the prepared bone. These channels enter the bone’s marrow cavity, which is filled with blood and special cells that can differentiate into cartilage-like cells (fibro-chondrocytes). After the procedure, the defect fills with a fibrous clot of blood, platelets, and fibrocytes. With the correct post-operative regimen, the clot can be “trained” to become even more like regular cartilage. Microfracture procedures are almost always done arthroscopically. (Figure 10a, Figure 10b, Video 2: microfracture) Osteoarticular Transplants: OATs During an OATs procedure, the diseased region of cartilage and its underlying bone are outlined and will be removed and replaced with donor cartilage and bone. For small lesions, (< 1cubic centimeter), the diseased cartilage is removed in a cylindrical core (called the “recipient site”) and replaced with a healthy cartilage-bone core from elsewhere in the knee (called the “donor site”). When lesions are large, a single core large enough to fill the recipient site cannot be safely harvested from elsewhere in the knee. There are two ways to address larger lesions:
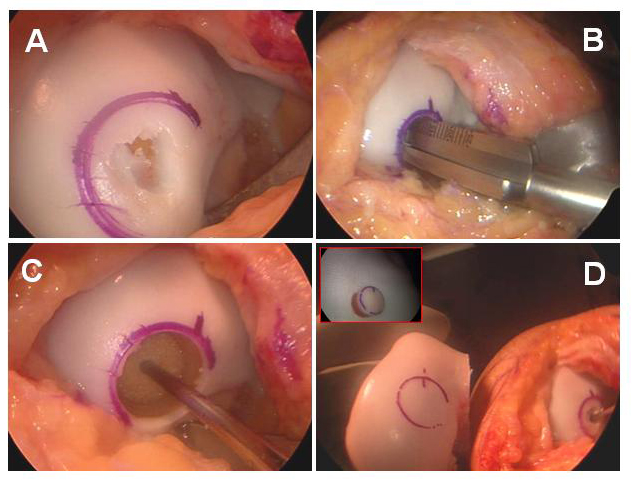
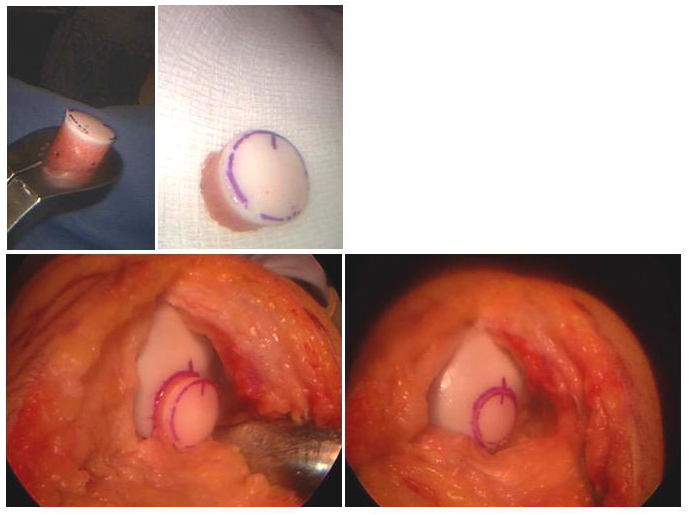
Once the bony plug of the OATs, mosaicplasty, or allgograft OATs heals in the socket (like healing a fracture), the overlying cartilage will transmit force more normally. Very small OATs plugs can be harvested and implanted arthroscopically, but larger lesions usually require a small incision. (Figure 11a, Figure 11b) Autologous Chondrocyte Implantation: ACI ACI is used to fill a defect that has normal underlying bone with cartilage-like cells. ACI requires two procedures. The first procedure is a diagnostic arthroscopy in which several (5 or 6) small rice-sized pieces of cartilage are removed from the knee. These are sent to a laboratory where the cells are cultured to become the precursor cells of cartilage tissues, called “chondrocytes”. These cells are then sent back to the surgeon in a small vial. The second procedure is done using open incisions. Like microfracture, the defect is prepared so that the surrounding shoulder of cartilage is normal—like a pothole in the road. Next, a flap of tissue removed from the nearby bone (called “periosteum”) is sewn directly over the recipient site to enclose the defect (like Saran wrap over a bowl). The grown chondrocytes are then injected beneath this cover or flap, where they will grow and mature into cartilage-like cells. The flapped, filled defect must be protected from trauma while the cells mature. (Figure 12) Meniscal Transplantation A meniscus is a c-shaped structure in the knee that is attached to the bone of the tibia at the front and back, and to the surrounding knee-joint capsule around the edge. This structure is critical to the function of the meniscus, so the bony attachments and soft-tissue attachments must be duplicated during replacement. During meniscal transplantation, the damaged remnants of the original meniscus are removed back to the attachment of the meniscus to the inside edge of the joint (called the capsule), and the front and back attachments are removed from the bone. A donor meniscus is used, and prepared in such a way that the donor’s bony attachments are preserved. These are left separate plugs (for medial meniscus transplants) or a dovetailed block. A matching dovetailed slot is created in the patient’s tibia, where the donor block will be inserted. In addition, the meniscus is sewn to the prepared capsule at its edges, re-establishing the bony and soft-tissue connections. Some time is required for the bone and soft-tissue to heal before the meniscus can be expected to function normally—during this time, the transplant must be protected. Unlike kidney, heart, lung, or liver transplants, allografts have relatively few viable cells, so there is rarely an immune response to them. No immuno-suppressive medications are required. (Figure 9, Video 3: meniscal transplantation) Osteotomies and Bone Realignment Osteotomy procedures are designed to correct abnormalities in the weight-bearing axis of bone. In general, the procedures involve taking or making a “wedge” out of the bone to re-align the extremity. This is like making a very controlled fracture of bone. These osteotomies can be made in the upper tibia (“high tibial osteotomy” or HTO) or at the far end of the femur (“distal femoral osteotomy”). The bone is held in the new alignment with plates and/or screws during the healing process. When the bone is healed, it will be in a position that changes the regions where force is concentrated within the joint. Another type of osteotomy can be made to change the direction of pull and force that the joint experiences between the patella and the femur. The indications for each type of osteotomy are beyond the scope of this review, and should be discussed with your surgeon. (Figure 13) Anesthetic Arthroscopic and traditional open knee procedures may be performed under a general anaesthetic or under a regional block that makes the knee and leg numb during and for several hours after the procedure. The patient may wish to discuss their preferences with the anesthesiologist prior to surgery. Length of microfracture, meniscal transplantation, osteoarticular allograft/autograft transplants (oats), autologous chondrocyte implantation (aci) and osteotomy for arthritis in the athlete. Depending on the complexity of the injury and treatment, the procedure takes approximately 2 to 6 hours to complete. Patients usually spend 1 or 2 hours in the recovery room. Patients who undergo arthroscopic procedures almost always are comfortable enough to be discharged home. Those undergoing more complex restorative procedures (osteotomies, ACI, massive OATs, or meniscal transplantation) will usually require at least one night’s hospitalization. Pain and pain management Recovery of comfort and function following cartilage restoration continues over a few months. Initially, the knee must be protected from overuse while it heals. A very strict rehabilitation program and, occasionally, a protective brace, can help with this healing. Ironically, many patients who undergo these procedures feel very comfortable long before the definitive healing has taken place, so strict adherence to limits on activity is critical. Immediately after surgery, the patient is given strong medications (such as morphine) to help with tissue pain and discomfort from swelling. Most patients are discharged with a prescription for oral pain medications (such as hydrocodone or Tylenol with codeine). Use of medications Immediately after surgery, pain medications are given through an intravenous (IV) line. Patients who require a hospital stay are placed on patient-controlled anesthesia (PCA) to allow them to administer their own medication as it is needed. Oral pain medications are rarely required after the first few weeks following the procedure. Effectiveness of medications Pain medications are very powerful and effective. Their proper use lies in the balancing of their pain-relieving effect and their other, less desirable effects. Good pain control is an important part of appropriate postoperative management. Important side effects Other pain medications (taken through the IV or orally) can cause drowsiness, slowness of breathing, difficulties in emptying the bladder or bowel, nausea, vomiting, itching, or allergic reactions. Patients who have been on pain medications for a long time prior to surgery may find that the usual doses of pain medication are less effective. For some patients, balancing the benefits and side effects of medications is challenging. Patients should notify their surgeon if they have had previous difficulties with pain medications or pain control. Hospital stay Some patients will require a hospital stay after a complex articular or meniscal cartilage restoration procedure. Prior to discharge from the hospital, detailed instructions for the care of their knee, activity restrictions, bathing, use of medications and potential problems are explained to the patient and their family prior to discharge. Recovery and rehabilitation in the hospital RECOVERY AND RECOUPERATION IN THE FIRST FEW WEEKS
Because fluid is used to expand the knee joint during arthroscopic procedures, the knee is frequently swollen for a day or so following surgery. Also, the incisions will “weep” fluid for a couple of days postoperatively, and the dressing can become damp. The patient is asked to refrain from weight bearing on a knee or ankle EVEN IF IT FEELS GOOD for 4 to 6 weeks after the procedure and remove the brace only to perform a strict set of limited exercises. These exercises will be explained prior to discharge. For the first 2 weeks, a home program of rest and limited self-therapy is usually recommended, including use of the CPM machine. Then, after the wounds have healed, the patient is referred to an experienced team of physical therapists, rehabilitation specialists, and athletic trainers to guide and monitor the rehabilitation. This is almost always possible on an outpatient basis. Physical therapy Early motion is critical after the articular cartilage procedures, but unrestricted motion can endanger the success of the procedure. For the first 2 weeks, the patient spends about 6-8 hours per day on the CPM machine to retain and regain motion. After the wounds have begun healing, the patient is scheduled to see a physical therapist twice or three times per week to monitor the progress of healing, teach the proper exercises, and guide the patient in a strengthening program. After two weeks, a more comprehensive rehabilitation program is started. During this period, the therapist works closely with the patient to re-establish a normal range of motion. The therapist and patient work together, but the patient is expected to do “homework” on a daily basis so that constant improvement is achieved. Once a normal range of motion is re-established, knee strengthening is started. It takes about 12 weeks before the knee is completely rehabilitated for the normal activities of daily living, and about 9 to 12 months before low-impact sports can be re-started. At our institution, we utilize athletic trainers to work with patients on “sports-specific” training to re-train the muscles and knee for golf, tennis, running, cutting, and swimming. Rehabilitation options The results of physical therapy are optimized by a competent therapist, familiar with the procedure and the usual expectations, and a compliant patient, who does home exercises and is motivated to improve. Most surgeons have a standard protocol that they can give to a physical therapist to let them know how to rehabilitate the knee. It is important for a patient to find a therapist with flexible hours and a convenient location because the therapy will become part of a routine for 4 to 9 months. The surgeon can recommend a therapist or therapy group with whom he or she is used to working and who is familiar with the procedure. Therapy is generally done on an outpatient basis, with 2 or 3 visits per week so that the therapist can check the progress and review or modify the program as needed to suit the individual. Usual response Patients are almost always satisfied with the range of motion, comfort, and function that they achieve as the rehabilitation program progresses. Some patients will lose a slight degree of knee motion (the ability to bring the heel to the buttock), but this does not usually interfere with daily activities or sports. Occasionally, the knee may retain a slight degree of discomfort with activities compared to the other knee, although this is usually minimal and does not require bracing. Alternatively, the knee can become stiff after surgery. Many patients are encouraged to return to non-impact athletics, such as cycling, swimming, climbing, cross-country skiing, snowshoeing, etc. Risks There are very few risks to appropriate postoperative therapy. If the therapist and surgeon do not communicate about what exactly what was done and what the short- and long-term expectations are following the procedure, the therapist can be too aggressive or too timid about the rehabilitation. This can result in mild knee stiffness or laxity. When the patient, physician, and rehabilitation specialist are in good communication regarding the timing and expectations of the rehabilitation process, the results are usually excellent. Duration of rehabilitation Every patient is slightly different. Once the range of motion is acceptable and the strength has returned, the rehabilitation program can be cut back to a minimal level. Patients who have special needs, such as cutting athletes, runners, and heavy laborers, may require sports-specific training or “work hardening” with a therapist or athletic trainer. Frequently, the surgeon will discourage heavy labor and impact or cutting athletics after the reconstruction of large cartilage defects. Returning to ordinary daily activities In general, patients are able to resume activities of daily living using crutches or a walker within 3 to 4 weeks after surgery if a weight-bearing joint (knee or ankle) is involved. Most persons who work at a desk job can return to work during this time. The patient is strongly encouraged to avoid weight-bearing at all times for the first 6 to 8 weeks. After this time, the patient is gradually advanced to full weight bearing. Athletics are discouraged until about 9 months post-op. Driving should wait until the patient can perform the necessary functions comfortably and confidently, pain is at a minimum, and pain medications are not required. A good question to ask a patient is, “Would you want you driving if your 4-year old child was in the car or playing in the street?” In general, it may take longer for a person to drive after the right knee has undergone surgery because of the increased demands on the right leg for driving. With the consent of their surgeon, a patient may return to activities such as swimming and golf between 4 and 6 months following the procedure. More extreme sports (wrestling, running, hiking on uneven ground, soccer, basketball, etc) should only be undertaken after at least 9 months of rehabilitation, when the knee is extremely comfortable and the strength is 90 percent of the uninjured knee. Such sports may be discouraged by your surgeon. Long-term patient limitations After the appropriate procedure and a comprehensive rehabilitation have been completed, most patients can return to work and non-impact athletics without disability. Depending on the procedures performed, concomitant injuries, and the stability of the knee, many patients will choose to return to cutting athletics such as basketball, football, or skiing. Costs The surgeon and therapist should provide the information of the usual cost of the rehabilitation program. Most insurance policies will cover the costs of some or most of the rehabilitation. Careful adherence to at-home exercises between visits will usually decrease the overall number and frequency of visits required. Summary of microfracture, meniscal transplantation, osteoarticular allograft/autograft transplants (oats), autologous chondrocyte implantation (aci) and osteotomy for arthritis in the athlete. for arthritis, osteochondral defects (ocd lesions), meniscus transplantation and cartilage loss in the knee. THE FIVE THINGS ONE NEEDS TO KNOW ABOUT THE TREATMENT ARTICULAR CARTILAGE DEFECTS AND MENISCAL REPLACEMENT:
|