Two options: total shoulder and ream and run
 Edited by: Matthew D. Saltzman, M.D., and Frederick A. Matsen III, M.D., Professor, UW Orthopaedics & Sports Medicine
Edited by: Matthew D. Saltzman, M.D., and Frederick A. Matsen III, M.D., Professor, UW Orthopaedics & Sports MedicineLast updated: December 12, 2013
Follow our blog
http://shoulderarthritis.blogspot.com/
On which we try to provide the best and most current information on shoulder arthritis.
To read more about Shoulder Arthritis, please visit our online Shoulder Arthritis Book.
Contact
If you have questions regarding the ream and run procedure feel free to email Frederick A. Matsen III M.D. at matsen@uw.edu.
Summary
Joint replacement surgery is the most reliable solution for patients with shoulder arthritis that causes disabling pain and loss of function. The two types of replacement surgery for patients that have arthritis that affects both the ball (humerus) and socket (glenoid) are: (1) Total Shoulder Arthroplasty and (2) ‘Ream and Run’. The following Frequently Asked Questions are intended to help you decide which is best for you.
JBJS Article for Self-Assessed Outcome After Shoulder Hemiarthroplasty (PDF) (0.78 MB)
Article on Nonprosthetic Glenoid Arthroplasty (PDF) (0.09 MB)
Article for 282 unsatisfactory shoulder arthroplasties (PDF) (0.09 MB)
JBJS Article on Total Shoulder Arthroplasty (PDF)(2.01 MB)
Total Shoulder Arthroplasty involves replacement of the worn out ball with a smooth metal ball. This ball is connected to a metal stem that is placed on the inside of your arm bone (humerus) [FIGURE 1]. The stem is held in place with some of your own bone that is taken from the ball (humeral head). The socket (glenoid) component is made out of plastic and is held in place with a small amount of bone cement [FIGURE 2]. The final replacement consists of a smooth metal ball moving on a smooth plastic socket. [FIGURES 3 4 5 & 6]
Click to enlarge

FIGURE 1: Humeral component that is used for both Total Shoulder Arthroplasty and the Ream and Run procedure. The stem is titanium and the ball is metal alloy.
Click to enlarge

FIGURE 2: Glenoid component that is used for Total Shoulder Arthroplasty only. It is made of a plastic known as polyethylene.
Click to enlarge

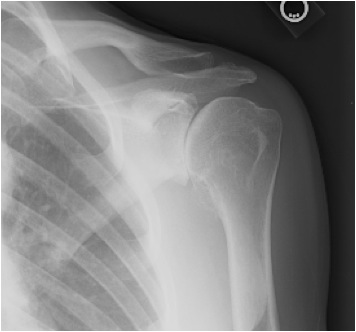
FIGURES 3: X-rays of a 58 year-old woman with severe osteoarthritis of the shoulder. Note the large bone spurs and absence of joint space.
Click to enlarge

FIGURES4: X-rays of a 58 year-old woman with severe osteoarthritis of the shoulder. Note the large bone spurs and absence of joint space.
Click to enlarge
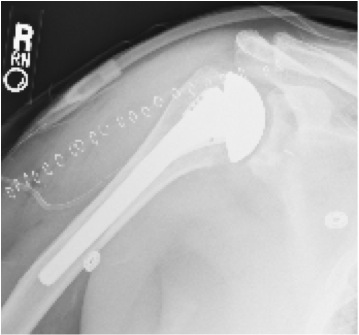
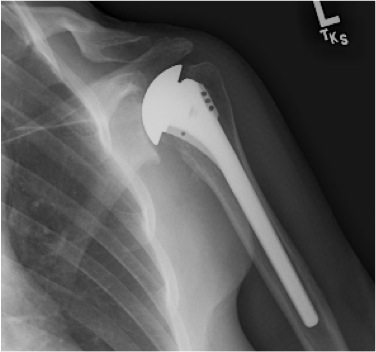
FIGURES 5: X-rays of the same woman in Figures 3 & 4 after Total Shoulder Arthroplasty. Note that the bone spurs have been removed and that the humeral component has been placed inside of the arm bone. The plastic glenoid component is not visible on x-ray.
Click to enlarge
FIGURES 6: X-rays of the same woman in Figures 3 & 4 after Total Shoulder Arthroplasty. Note that the bone spurs have been removed and that the humeral component has been placed inside of the arm bone. The plastic glenoid component is not visible on x-ray.
Not all surgical cases are the same, this is only an example to be used for patient education.
Who should consider Total Shoulder Arthroplasty?
Individuals who want the quickest and most reliable path to a comfortable shoulder should strongly consider Total Shoulder Arthroplasty. Resurfacing the ball with metal and the socket with plastic provides an immediate smooth surface for your shoulder. This means that your shoulder should be quite comfortable within weeks following the surgery. Although daily exercises are still encouraged they do not have to be quite as rigorous as in individuals who opt for the Ream and Run surgery. If you anticipate having difficulty doing exercises multiple times per day for several months total shoulder arthroplasty may be a better option for you. Additionally individuals who live sedentary lifestyles smokers diabetics and those who require heavy narcotics for shoulder or other pain are generally better off with a total shoulder arthroplasty than a Ream and Run procedure.
What is the 'Ream and Run' procedure?
The Ream and Run procedure involves replacement of the worn out ball with a smooth metal ball that is connected to a metal stem just like in the total shoulder (below). The stem is placed inside of the arm bone (humerus) and held in place with some of your own bone that is taken from the ball (humeral head). The main difference between a ‘Ream and Run’ and a Total Shoulder Arthroplasty is that with the ‘Ream and Run’ a plastic glenoid component and bone cement are not needed. Instead the socket (glenoid) is ground down so that it is a smooth shallow cup – a shape that resembles that of the normal socket [FIGURES 7 & 8]. The final replacement consists of a smooth metal ball moving on smooth socket bone. [FIGURES 9 10 11 & 12] The grinding process allows bone cells to come to the surface of the socket. These cells can form a new surface that is very similar to the cartilage that normally covers the socket however this process can take 3 to 12 months to occur.
Click to enlarge
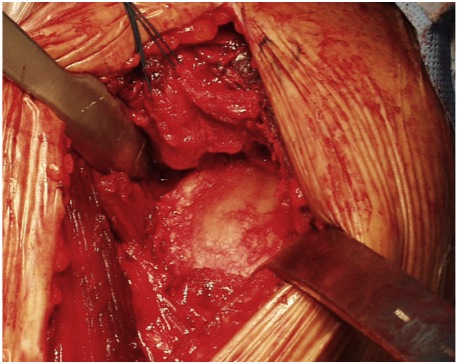
FIGURE 7: The socket (glenoid) before it has been ground down. Note that nearly all of the normal cartilage has been worn away by the disease process.
Click to enlarge
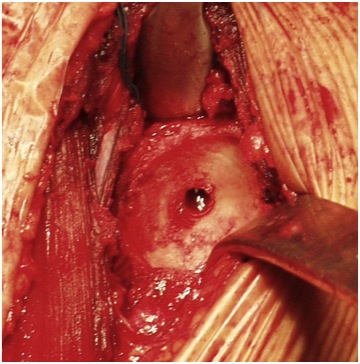
FIGURE 8: The socket (glenoid) after it has been ground down so that it is a smooth shallow cup. Note the bleeding bone that will bring in cells to form a new cartilage-like layer.
Click to enlarge
FIGURES 9: X-rays of a very active 57 year-old woman with advanced arthritis of the shoulder. Note the bone spurs and absence of joint space.
Click to enlarge

FIGURES 10: X-rays of a very active 57 year-old woman with advanced arthritis of the shoulder. Note the bone spurs and absence of joint space.
Click to enlarge
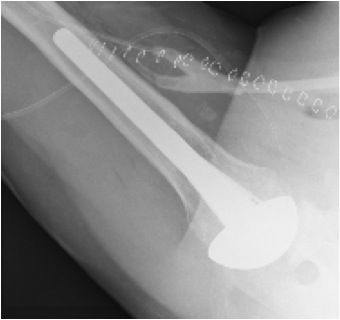
FIGURES 11: X-rays of the same woman in Figures 9 & 10 after the Ream and Run procedure. Note that the bone spurs have been removed and that the humeral component has been placed inside of the arm bone. Figure 12 shows space between the metal ball and socket that implies that a new cartilage-like surface has formed.
FIGURES 12: X-rays of the same woman in Figures 9 & 10 after the Ream and Run procedure. Note that the bone spurs have been removed and that the humeral component has been placed inside of the arm bone. Figure 12 shows space between the metal ball and socket that implies that a new cartilage-like surface has formed.
Who should consider Ream and Run?
Individuals who enjoy strenuous activities such as weightlifting, waterskiing, contact sports, landscaping and chopping wood should strongly consider having a Ream and Run procedure. These activities put a lot of stress on the shoulder joint. Over time these stresses can wear out or loosen the plastic socket of a Total Shoulder Arthroplasty. If this occurs it may be necessary to have another surgery to remove the plastic component. Individuals less than 50 years old may wear out or loosen the plastic glenoid component even with less strenuous activities so they too should consider having a Ream and Run instead of Total Shoulder Arthroplasty.
What aspects of shoulder replacement surgery are the same for Total Shoulder Arthroplasty and Ream and Run?
Regardless of which of the two procedures you choose to have certain aspects of the surgery will be the same. An incision is made across the front of the shoulder from the collarbone to the middle of the arm bone so that the surgeon can gain access to the shoulder without having to cut either the deltoid or the pectoralis major muscles. One of the four rotator cuff tendons needs to be released to access the shoulder joint. This tendon (the subscapularis) is repaired at the end of the surgery and takes 3 months to completely heal back to the bone. The tight soft tissues and bone spurs that have formed as a result of the arthritis need to be released and removed for both procedures.
The metal ball and the stem that is attached to it are the same for both procedures. In both cases the stem is held in place inside your arm bone by bone that has been removed from the arthritic portion of the ball. This bone supports the metal ball and stem in the proper position.
For either procedure you usually have a choice of a general anesthetic or a brachial plexus block for your surgery. The block completely numbs your arm for approximately 12 hours and thus helps keep you comfortable immediately following surgery. When the block wears off the pain comes back and needs to be managed with medication given by mouth or in the IV.
Both procedures take approximately 2 hours to complete. Typically you will stay in the hospital for 2 nights regardless of which procedure you have done. Your rehabilitation exercises will start the evening of surgery or the very next morning. The exercises that you do are the same regardless of which procedure you have done. However the Ream and Run procedure requires a very strong dedication to the exercises as your shoulder is more likely to get stiff following this procedure than Total Shoulder Arthroplasty.
After either procedure there may be bleeding into the shoulder from cutting the bone. Bone is not in fact ‘dry as a bone’ but has many small blood vessels in it that may leak a bit after surgery. Often a drain is used for a day after surgery to remove this blood.
A study performed here at University of Washington showed Total Shoulder Arthroplasty and Ream and Run are equally likely to provide patients with a comfortable and functional shoulder. Article on Nonprosthetic Glenoid Arthroplasty (PDF) (0.09 MB).
What aspects of shoulder replacement surgery are different for Total Shoulder Arthroplasty and Ream and Run?
The main difference between the two procedures is in the work that is done on the socket. In Total Shoulder Arthroplasty the socket is resurfaced with a plastic component that is cemented into your bone. In the Ream and Run no plastic or cement used. Instead the socket is ground down so that it is smooth and will mate with the smooth metal ball. The ground down bone bleeds and this bleeding allows bone cells to cover the surface of the socket. Over time these cells form what is known as fibrocartilage which is similar but not the same as the cartilage that covers the socket in normal shoulders.
While patients who undergo Ream and Run may ultimately achieve the same level of comfort and function as those who undergo Total Shoulder Arthoplasty it may take some patients longer to reach this level. Some patients achieve it just as quickly as those who undergo Total Shoulder Arthroplasty some take up to 12 months to achieve this level and a few never achieve the same level of comfort that they would with Total Shoulder Arthroplasty. Article on Nonprosthetic Glenoid Arthroplasty (PDF) (0.09 MB).
Because the Ream and Run relies on the bone cells to form fibrocartilage certain individuals are not good candidates for the procedure. Smokers and patients with diabetes do not have the robust bone cells that are necessary for this healing to take place and are thus better off with a Total Shoulder Arthroplasty
What happens if my Total Shoulder Arthroplasty fails?
The most likely way that Total Shoulder Arthroplasty fails is by loosening or wear of the plastic glenoid component. If this occurs a second surgery is necessary to remove the loose component. It is usually not possible to place a new plastic component because there is typically not enough bone remaining to support it. If that is the case we usually try to smooth the remaining bone so that it can accommodate the metal ball. Surprisingly many patients have very good comfort and function following such an operation.
What happens if my Ream and Run fails?
Although most patients have very good return of comfort and function to their shoulder following the Ream and Run a few never get the type of pain relief that they had hoped for. It is difficult to predict who will fall into this category but in our experience it is fewer than 1 in 20 patients. These patients are often those who found it difficult to maintain their range of motion after surgery. It is possible to go in via a second surgery either to release the soft tissues to restore the range of motion or to place a plastic glenoid component in essence converting the Ream and Run to a Total Shoulder Arthroplasty. Most of the work has already been done with the first operation so the recovery is not quite as long as with the first surgery.
What are the most likely ways in which my shoulder replacement could fail?
Loosening of the plastic glenoid component is the most likely way that total shoulder arthroplasty fails. Pain and stiffness are the most common symptoms associated with such failure. Less common symptoms are: weakness instability infection and fracture.
Article for 282 unsatisfactory shoulder arthroplasties (PDF) (0.09 MB)
JBJS Article on Total Shoulder Arthroplasty (PDF)(2.01 MB) How long do shoulder replacements last?
It is difficult to know how long shoulder replacements will hold up for. It is largely dependent on how the shoulder is used. Patients who participate in activities that place a large amount of stress on the shoulder may wear out the components sooner than those who are less vigorous with their shoulders. The materials that current shoulder replacement components are made out of (metal alloy humeral head titanium humeral stem and highly crosslinked polyethylene glenoid component) are much better than their predecessors twenty years ago. Modern shoulder replacements will likely last for at least 15-20 years as long as the limitations imposed by the surgeon are respected. When do I need to decide whether I will have a Total Shoulder Arthroplasty or Ream and Run?
Most patients choose which procedure they would like to have prior to the day of surgery. Occasionally a patient will change their mind the morning of surgery. We can usually accommodate their request as our surgical team performs several of both procedures each day and we therefore have the equipment and personnel available to perform either procedure.
What do I do if I have questions that are not answered?
It is very important that all your questions be answered before surgery. You should have phone and email contact information for your surgeon. Be sure to ask! I live a long way from the Hospital; how will I keep in touch and how often do I have to come back?
We encourage all of our patients to keep in touch once they leave the hospital. You will be given email addresses and phone numbers of the entire Shoulder and Elbow Team. We welcome any and all questions and encourage you to let us know about even the most minor concerns. Typically we see you back at 2 weeks following surgery for removal of the skin staples 6 weeks for x-rays and advancement of physical therapy and then at 3 months 6 months and 1 year thereafter. Patients who live far from Seattle may prefer to have their local doctor remove the skin staples at 2 weeks following the surgery. This is fine as long as you let us know about any concerns you or your doctor have along the way. Will I need formal physical therapy after my surgery?
In most cases patients do not require formal physical therapy following shoulder replacement surgery. Our Shoulder Therapist will spend several sessions with you while you are in the hospital. It is our hope that you will feel comfortable performing the exercises on your own. The exercises are simple in nature and we have found that most patients enjoy being in charge of their own rehabilitation. [FIGURE 13] If you have concerns over your range of motion at any point during your recovery we would like to know immediately. Some patients prefer to see a physical therapist on a regular basis following discharge from the hospital. If this is your preference please let us know and we will make appropriate arrangements.
Click to enlarge

FIGURE 13: A patient doing self-directed exercises following shoulder replacement surgery.
Will I need pain medications and if so who will give them to me?
Every patient is different as far as how much and what type of pain medication they require after shoulder replacement surgery. We will work closely with you while you are in the hospital to find the right regimen for you. You will be given prescriptions for all the medications that you require prior to discharge. We have found that the sooner patients get off narcotics following surgery the smoother their recovery is. If the pain medications that you leave the hospital are not working or if you need a refill please contact our clinic nurse. Acetaminophen (Tylenol) is ‘ok’ to take immediately following surgery as long as you don’t exceed the maximum daily dose (4000mg) and nonsteroidal anti-inflammatories (ibuprofen naproxen Advil Motrin Aleve) are ‘ok’ to take 6 weeks following your surgery.
Will X-rays be taken after my surgery?
X-rays are taken immediately following surgery and then again at your 6 week visit. We will typically get x-rays at the 3 month 6 month and 1 year visit as well.
How will I know if I am on the right track after my surgery?
Your shoulder should continue to get more comfortable each day following surgery. We ask that you keep track of your range of motion when you do your exercises. You are on the right track if you continue to gain range of motion. If at any point you start to loose motion you may be off the right track and we ask that you contact us immediately.
127
