Last updated: Monday, January 28, 2013
Quotes
"It deserves to be known how a shoulder which is subject to frequent dislocations should be treated. For many persons owing to this accident have been obliged to abandon gymnastic exercises though otherwise well qualified for them; and from the same misfortune have become inept in warlike practices and have thus perished. And this subject deserves to be noticed because I have never known any physician (to) treat the case properly; some abandon the attempt altogether and others hold opinions and practice the very reverse of what is proper."
- Hippocrates 2400 years ago
"In every case the anterior margin of the glenoid cavity will be found to be smooth rounded and free of any attachments and a blunt instrument can be passed freely inwards over the bare bone on the front of the neck of the scapula."
- Perthes 1906
"...the only rational treatment is to reattach the glenoid ligament (or the capsule) to the bone from which it has been torn."
- Bankart 1939 (Bankart 1939)
Shoulder stabilization surgery usually can be accomplished through cosmetically acceptable incisions in the lines of the skin.
Placement of incision
Anteriorly the surgeon can identify and mark the prominent anterior axillary crease by adducting the shoulder. An incision placed in the lower part of this crease provides excellent access to the shoulder for anterior repair and yet heals nicely with a subcuticular closure. When cosmesis is a concern the incision can be made more into the axilla as described by Leslie and Ryan. (Leslie and Ryan 1962)
Posteriorly an analogous vertical incision in line with the extended posterior axillary crease (best visualized by extending the shoulder backwards) also heals well. Fortuitously these creases lie directly over the joint to which the surgeon needs access.
The shoulder is covered by the deltoid muscle arising from the clavicle acromion and scapular spine.
Anatomy of the deltoid
The anterior deltoid extends to a line running approximately from the midclavicle to the midlateral humerus. This line passes over the cephalic vein the anterior venous drainage of the deltoid and over the coracoid process. The deltoid is innervated by the axillary nerve whose branches swoop upward as they extend anteriorly. The commonly described "safe zone" 5 cm distal to the acromion does not take into account these anterior branches which may come as close as 2 cm to the acromion. At the deltopectoral groove the deltoid meets the clavicular head of the pectoralis major which assists the anterior deltoid in forward flexion. The medial and lateral pectoral nerves are not in the surgical field of shoulder stabilization. Splitting the deltopectoral interval just medial to the cephalic vein preserves the deltoid's venous drainage and takes the surgeon to the next layer. It is important to note that extension of the shoulder tightens the pectoralis major and the anterior deltoid as well as the coracoid muscles compromising the exposure. Thus assistants must be reminded to hold the shoulder in slight flexion to relax these muscles and facilitate access to the joint.
Posteriorly the medial edge of the deltoid is too medial to provide useful access to the glenohumeral joint. Access must be achieved by splitting the deltoid which is most conveniently done at the junction of its middle and posterior thirds. This junction is marked by the posterior corner of the acromion. The site is favorable for a split because it overlies the joint and also because the axillary nerve exiting the quadrangular space divides into two trunks (its anterior and posterior branches) near the inferior aspect of the split.
The coracoid process is the "lighthouse" of the anterior shoulder providing a palpable guide to the deltopectoral groove a locator for the coracoacromial arch and an anchor for the coracoid muscles (the coracobrachialis and short head of the biceps) that separate the lateral "safe side" from the medial "suicide" where the brachial plexus and major vessels lie.
The coracoid process
The surgeon comes to full appreciation of the value of such a lighthouse when it is lacking--for example when re-exploring a shoulder for complications of a coracoid transfer procedure. The clavipectoral fascia covers the floor of the deltopectoral groove. Rotating the humerus enables the surgeon to identify the subscapularis moving beneath this fascial layer. Incising the fascia up to but not through the coracoacromial ligament preserves the stabilizing function of the coracoacromial arch.
Location of gliding
The humeroscapular motion interface (see figures 1 and 2) separates the structures that do not move on humeral rotation (the deltoid coracoid muscles acromion and coracoacromial ligament) from those that do (the rotator cuff long head of the biceps tendon and humeral tuberosities). During shoulder motion substantial gliding takes place at this interface (see figure 3). The humeroscapular motion interface provides a convenient plane for medial and lateral retractors and is also the plane in which the principal nerves lie.
The axillary nerve runs in the humeroscapular motion interface superficial to the humerus and cuff and deep to the deltoid and coracoid muscles (see figure 4). Sweeping a finger from superior to inferior along the anterior aspect of the subscapularis muscle catches the axillary nerve hanging like a watch chain across the muscle belly. Tracing this nerve proximally and medially leads the finger to the bulk of the brachial plexus. Tracing it laterally and posteriorly leads the finger beneath the shoulder capsule toward the quadrangular space. From a posterior vantage the axillary nerve is seen to exit the quadrangular space beneath the teres minor and extending laterally where it is applied to the deep surface of the deltoid muscle. By virtue of its prominent location in close proximity to the shoulder joint anteriorly inferiorly and posteriorly the axillary nerve is the most frequently injured structure in shoulder surgery.
The musculocutaneous nerve lies on the deep surface of the coracoid muscles and penetrates the coracobrachialis with one or more branches lying a variable distance distal to the coracoid. (The often-described 5 cm "safe zone" for the nerve beneath the process refers only to the average position of the main trunk and not to an area that can be entered recklessly.) The musculocutaneous nerve is vulnerable to injury from retractors placed under the coracoid muscles and to traction injury in coracoid transfer. Knowledge of the position of these nerves can make the shoulder surgeon both more comfortable and more effective.
The next layer of the shoulder is the rotator cuff.
Tendons of the rotator cuff
The tendons of these muscles blend in with the capsule as they insert to the humeral tuberosities (Clark and Harryman 1992). Thus in reconstructions that require splitting of these muscles from the capsule this splitting is more easily accomplished medially before the blending becomes complete. The nerves to these muscles run on their deep surfaces: the upper and lower subscapular to the subscapularis and the suprascapular to the supraspinatus and infraspinatus. Medial dissection on the deep surface of these muscles may jeopardize their nerve supply. (Yung and Harryman 1995)
The cuff is relatively thin between the supraspinatus and the subscapularis (the "rotator interval"). This allows the cuff to slide back and forth around the coracoid process as the arm is elevated and lowered. Splitting this interval toward the base of the coracoid may be helpful when mobilization of the subscapularis is needed.
The tendon of the long head of the biceps originates from the supraglenoid tubercle. It runs beneath the cuff in the area of the rotator interval and exits the shoulder beneath the transverse humeral ligament and between the greater and lesser tuberosities. It is subject to injury on incising the upper subscapularis from the lesser tuberosity. In the bicipital groove of the humerus this tendon is endangered by procedures that involve lateral transfer of the subscapularis tendon across the groove.
The glenohumeral joint capsule is normally large loose and redundant allowing for the full and free range of motion of the shoulder.
Redundancy
By virtue of their mandatory redundancy the capsule and its ligaments are lax throughout most of the range of joint motion. Thus they can exert major stabilizing effects only when they come under tension as the joint approaches the limits of its range of motion.
The three anterior glenohumeral ligaments were first described by Schlemm. (Schlemm 1853) Since then many observers have described their anatomy and their roles in limiting glenohumeral rotation and translation. (Delorme 1910; DePalma 1970; Ferrari 1990; Fick 1904; McLaughlin 1960; Moseley and Overgaard 1962; O'Connell et al 1990; Reeves 1968b; Turkel et al 1981; Weitbrecht 1969)
Codman (Codman 1934) and others pointed out the variability of the ligaments. (Delorme 1910; DePalma 1973; Ferrari 1990; Moseley and Overgaard 1962; O'Brien et al 1990b; Williams et al 1994) These authors also demonstrated a great variation in the size and number of synovial recesses that form in the anterior capsule above below and between the glenohumeral ligaments. They observed that if the capsule arises at the labrum there are few if any synovial recesses (in this situation there is a generalized blending of all three ligaments which leaves no room for synovial recesses or weaknesses and hence the anterior glenohumeral capsule is stronger). However the more medially the capsule arises from the glenoid (i.e. from the anterior scapular neck) the larger and more numerous are the synovial recesses. The end result is a thin weak anterior capsule. Uhthoff and Piscopo (Uhthoff and Piscopo 1985) demonstrated in an embryological study that in 52 specimens the anterior capsule inserted into the glenoid labrum in 77 per cent and into the medial neck of the scapula in 23 per cent.
The superior glenohumeral ligament (SGHL) is identified as the most consistent capsular ligament. (DePalma et al 1949) It crosses the rotator interval capsule lying between the supraspinatus and subscapularis tendons. Another interval capsular structure the coracohumeral ligament (CHL) originates at the base of the coracoid blends into the cuff tendons and inserts into the greater and lesser tuberosities. (Clark et al 1990; Harryman et al 1992; Jerosch et al 1990; Kuboyama 1991; Ovesen and Nielsen 1985a; Steiner and Hermann 1989)
Harryman et al have pointed out that these two ligaments and the rotator interval capsule come under tension with glenohumeral flexion extension external rotation and adduction. (Harryman et al 1992) When they are under tension these structures resist posterior and inferior displacement of the humeral head. Clinical and experimental data have shown that releasing or surgically tightening the rotator interval capsule increases or decreases the allowed posterior and inferior translational laxity respectively. (Basmajian and Bazant 1959; Harryman et al 1992; Neer et al 1989; Nobuhara and Ikeda 1987; Warner et al 1992)
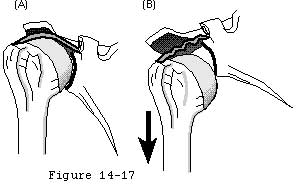
It is these ligaments and capsule as well as the inferior glenoid lip that provide static restraint against inferior translation. (Basmajian and Bazant 1959) It is of anatomical interest and clinical significance that when the lateral scapula is allowed to droop inferiorly the resulting passive abduction of the humerus relaxes the rotator interval capsule and the superior ligaments; as a result the humeral head can be "dumped" out of the glenoid fossa (see figure 5). (Matsen et al 1994) Drooping of the lateral scapula is normally prevented by the postural action of the scapular stabilizers particularly the trapezius and serratus. Elevation of the lateral scapula with the arm at the side enhances inferior stability in two ways: the resulting glenohumeral adduction tightens the superior capsule and ligaments and secondly the scapular rotation places more ofthe inferior glenoid lip beneath the humeral head. (Itoi et al 1992; Warner et al 1992)
While the SGHL and CHL come under tension with external rotation in adduction the middle glenohumeral ligament (MGHL) is tensioned by external rotation when the humerus is abducted to 45 degrees. (Symeonides 1972; Terry 1991; Turkel et al 1981) The MGHL originates antero-superiorly on the glenoid and inserts mid-way along the anterior humeral articular surface adjacent to the lesser tuberosity. In over a third of shoulders the MGHL is absent or poorly defined a situation which may place the shoulder at greater risk for anterior glenohumeral instability. (Morgan 1992)
With greater degrees of shoulder abduction for example in the "apprehension" position the inferior glenohumeral ligament (IGHL) and the inferior capsular sling come into play. (O'Connell et al 1991; Terry Hammon and France 1991; Turkel et al 1981) The IGHL originates below the sigmoid notch and courses obliquely between the antero-inferior glenoid and its humeral capsular insertion. (O'Brien et al 1990a) O'Brien et al have described an anterior thickening of the IGHL the anterior superior band.(O'Brien et al 1990a) The anterior and posterior aspects of the IGHL are said to function as a cruciate construct alternatively tightening in external or internal rotation. (O'Brien et al 1990a; Warner et al 1992; Warren 1984)
When the humerus is elevated anteriorly in the sagittal plane (flexion) the posterior-inferior capsular pouch along with the rotator interval capsule come into tension. (Harryman et al 1990; Harryman et al 1992; O'Brien et al 1990a; Rhee et al 1994; Warner et al 1992) If the humerus is internally rotated while elevated in the sagittal plane the interval capsule slackens but the posterior inferior pouch tightens. Posterior-inferior capsular tension also limits flexion internal rotation and horizontal adduction. (Harryman et al 1990; Harryman et al 1992; Rhee et al 1994) Excessive tightness of this portion of the capsule is a well-recognized clinical entity.
The glenoid labrum is a fibrous rim that serves to deepen the glenoid fossa and allow attachment of the glenohumeral ligaments and the biceps tendon to the glenoid.
Interconnection and anatomy
Anatomically it is the interconnection of the periosteum of the glenoid the glenoid bone the glenoid articular cartilage the synovium and the capsule. While microscopic studies have shown that a small amount of fibrocartilage exists at the junction of the hyaline cartilage of the glenoid and fibrous capsule; the vast majority of the labrum consists of dense fibrous tissue with a few elastic fibers. (Gardner 1963; Moseley and Overgaard 1962; Townley 1950) The posterior-superior labrum is continuous with the long head tendon of the biceps. Anteriorly it is continuous with the inferior glenohumeral ligament. (Grant 1972; Moseley 1945; Moseley 1972; Trillat and Leclerc-Chalvet 1973) Hertz et al (Hertz et al 1986) detailed the micro anatomy of the labrum while Prodromos et al (Prodromos et al 1990) DePalma (DePalma 1973) and Olsson (Olsson 1953) have described the changes in the glenoid labrum with age.
In cadavers isolated labral deficiency is not usually sufficient to allow glenohumeral dislocation. (Pagnani et al 1995; Reeves 1968a; Reeves 1969; Townley 1950) However clinical studies reveal a high incidence of labral deficiency in recurrent traumatic instability. (Bankart 1939; D'Angelo 1970; DePalma 1950b; Matsen and Thomas 1990; Rowe et al 1978; Ungersbock et al 1995)
The reader is referred to a recent review of the gross anatomy of the glenohumeral joint surfaces ligaments labrum and capsule by Warner. (Matsen et al 1993)