The history should define the mechanism of the injury including the position of the arm the amount of applied force and the point of force application. (Protzman 1980; Rowe and Zarins 1981; Rowe and Zarins 1982)
Importance of history
Injury with the arm in extension abduction and external rotation favors anterior dislocation. Electroshock seizures or a fall on the flexed and adducted arm are commonly associated with posterior dislocation. If the instability is recurrent the history defines the initial injury the position or action which results in instability how long the shoulder stays "out whether radiographs are available with the shoulder out of joint, and what means have been necessary to reduce the shoulder. The history also solicits evidence of neurological or rotator cuff problems after previous episodes of shoulder instability. Previous treatment for the recurrent instability as well as the effectiveness of this treatment are documented.
Anterior dislocation
The acutely dislocated shoulder is usually very painful. Muscles are in spasm in an attempt to stabilize the joint. The humeral head may be palpable anteriorly. The posterior shoulder shows a hollow beneath the acromion. The arm is held in slight abduction and external rotation. Internal rotation and adduction are usually limited. Because of the frequent association of nerve injuries (de Laat et al 1994) and to a lesser extent vascular injuries (Blom and Dahlback 1970) an essential part of the physical examination of the anteriorly dislocated shoulder is the assessment of the neurovascular status of the upper extremity and the charting of the findings prior to reduction.
Posterior disclocation
Recognition of a posterior dislocation may be impaired by the lack of a striking deformity of the shoulder and by the fact that the shoulder is held in the traditional sling position of adduction and internal rotation. However a directed physical examination will reveal the diagnosis. The classical features of a posterior dislocation include:
- Limited external rotation of the shoulder (often to less than zero degrees).
- Limited elevation of the arm (often to less than 90 degrees).
- Posterior prominence and rounding of the shoulder compared with the normal side.
- Flattening of the anterior aspect of the shoulder.
- Prominence of the coracoid process on the dislocated side.
Asymmetry of the shoulder contours can often be best visualized by viewing the shoulders from above while standing behind the patient.
The motion is limited because the head of the humerus is fixed on the posterior glenoid rim by muscle forces or the head may actually be impaled on the glenoid rim. With the passage of time the posterior rim of the glenoid may further impact the fracture of the humeral head and produce a deep hatchet-like defect or V-shaped compression fracture which engages the head even more securely. Patients with old unreduced posterior dislocations of the shoulder may have 30 to 40 degrees of glenohumeral abduction and some humeral rotation owing to enlargement of the groove. With long-standing disuse of the muscles about the shoulder atrophy will be present which accentuates the flattening of the anterior shoulder the prominence of the coracoid and the fullness of the posterior shoulder.
Proper physical examination is essential. Rowe and Zarins (Rowe and Zarins 1982) reported 23 cases of unreduced dislocation of the shoulder of which 14 were posterior. Hill and McLaughlin (Hill and McLaughlin 1963) reported that in their series the average time from injury to diagnosis was eight months. In the interval before the diagnosis of posterior dislocation of the shoulder is made the injury may be misdiagnosed as a "frozen shoulder" (Hill and McLaughlin 1963; McLaughlin 1963a; McLaughlin 1963b) for which vigorous therapy may be mistakenly instituted in an attempt to restore the range of motion.
Radiographs
When a shoulder is dislocated radiographs need to demonstrate:
- The direction of the dislocation
- The existence of associated fractures (displaced or not) and
- Possible barriers to relocation.
The glenohumeral joint is most reliably imaged using three standardized views referred to the plane of the scapula: an anteroposterior view in the plane of the scapula (figure 1) a scapular lateral (figure 2) and an axillary view (figure 3). The complete series of three views oriented to the scapula provide much more information than the commonly obtained view in the plane of the body (figure 4). McLaughlin has said that the reliance on anteroposterior radiographs will lead the unwary orthopedist into a "diagnostic trap." (McLaughlin 1952) Dorgan (Dorgan 1955) reported that in addition to obesity technical factors may prevent accurate identification of the glenohumeral joint in the transthoracic lateral view.
Anteroposterior view in the plane of the scapula
In 1923 Grashey (Grashey 1923) recognized that in order to take a true anteroposterior radiograph of the shoulder joint the direction of the x-ray beam must be perpendicular to the plane of the scapula. This view is most easily accomplished by placing the scapula flat on the cassette (a position the patient can help achieve) and passing the x-ray beam at right angles to this plane centering it on the coracoid process (figure 5). This view can be taken with the arm in a sling; with the body rotated to the desired position. In the normal shoulder this view reveals a clear separation of the humeral subchondral bone from that of the glenoid (figure 5).
Lateral view in the plane of the scapula
This view is taken at right angles to the anteroposterior in the plane of the scapula (figure 2). (McLaughlin 1952; McLaughlin 1963a; McLaughlin 1963b; Neer 1968; Rockwood 1984) Like the anteroposterior view it can be obtained by positioning the body without moving the dislocated shoulder. The radiographic beam is passed from medial to lateral parallel to the body of the scapula while the cassette is held perpendicular to the beam at the anterolateral aspect of the shoulder (figure 2). (Rockwood 1984) In this view the contour of the scapula projects as the letter "Y." (Rubin et al 1974) The downward stem of the Y is projected by the body of the scapula; the upper forks are projected by the coracoid process anteriorly and by the spine and acromion posteriorly. The glenoid is located at the junction of the stem and the two arms of the Y. In the normal shoulder the humeral head is at the center of the arms of the Y that is in the glenoid fossa. In posterior dislocations the head is seen posterior to the glenoid; in anterior dislocations the head is anterior to it.
Axillary view
In this view first described by Lawrence in 1915 (Lawrence 1915; Merrill 1975) the cassette is placed on the superior aspect of the shoulder. This view requires that the humerus be abducted sufficiently to allow the radiographic beam to pass between it and the thorax. Fortunately sufficient abduction can be achieved by gentle positioning of the dislocated shoulder or by modifications of the technique (figure 3 and figures 6 through 8). The axillary radiograph is critical in the evaluation of the dislocated shoulder: it not only reveals unambiguously the direction and magnitude of head displacement relative to the glenoid but also the presence and size of head compression fractures fractures of the glenoid and fractures of the humeral tuberosities. The axillary view may also be helpful in judging the bony competence and version of the glenoid fossa but the projection must be standardized to avoid misinterpretation.
In his text on radiographic positioning Jordan demonstrated the various techniques for obtaining axillary lateral views. (Jordan 1935) Cleaves (Cleaves 1941; Merrill 1975) and Teitge and Ciullo (Post 1978) have described variations on this view (figure 8). Rockwood has pointed out that in the situation when the patient cannot abduct the arm sufficiently a curved cassette or a rolled cardboard cassette can be placed in the axilla and the radiographic beam passed from a superior position (figure 6). Bloom and Obata (Bloom and Obata 1967) have modified the axillary technique so that the arm does not have to be abducted (figure 7). They call this the Velpeau axillary lateral view. While wearing a sling or Velpeau dressing the patient leans backward 30 degrees over the cassette on the table. The x-ray tube is placed above the shoulder and the beam projected vertically down through the shoulder onto the cassette.
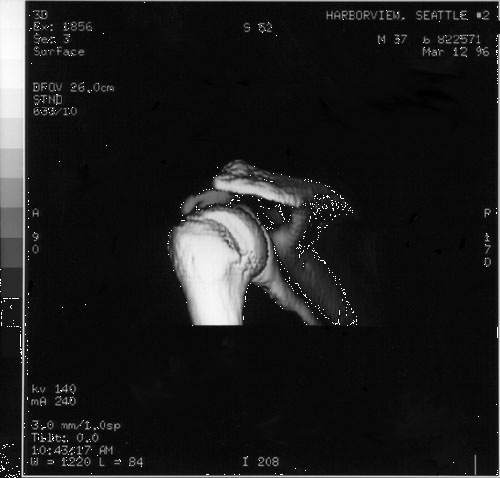
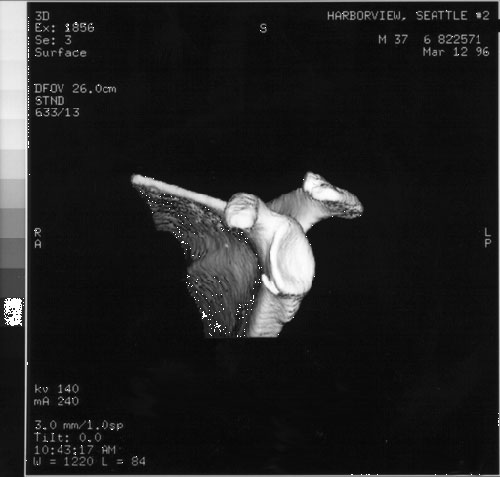
In summary in the evaluation of a possibly dislocated shoulder or a fracture-dislocated shoulder we recommend the three orthogonal projections of the shoulder (anteroposterior and lateral in the plane of the scapula and axillary views) which provide a sensitive assessment of shoulder dislocation. The use of fewer views or other less interpretable projections may obscure significant pathological processes. If the three views cannot be taken if there is a question regarding the diagnosis or if there is a need to define anatomy in greater detail a CT scan may be of great assistance. (Kinnard et al 1984; Ribbans et al 1990; Shuman et al 1983) Using modern methods of three dimensional reconstruction anterior inferior glenoid lesions and posterior lateral humeral head lesions can be shown in striking detail (figures 9 and 10). It is of note that the patient whose shoulder is shown in these figures obtained an excellent result from non operative treatment in spite of the damage shown on the reconstructions.