New Quad Sparing Technique May Provide Faster Recovery for Patients with Arthritis of the Knee

Edited by Seth S. Leopold, M.D., Professor, UW Orthopaedics & Hip & Knee
Overview
Knee replacement is a surgical procedure that decreases pain and improves the quality of life in many patients with severe knee arthritis. Typically patients undergo this surgery after non-operative treatments (such as activity modification anti-inflammatory medications or knee joint injections) have failed to provide relief of arthritic symptoms. Surgeons have performed knee replacements for over three decades generally with excellent results; most reports have ten-year success rates in excess of 90 percent.
Broadly speaking there are two types ways to insert a total knee replacement: the traditional approach and the newer minimally-invasive (sometimes called quadriceps-sparing) approach.
Traditional total knee replacement involves a roughly 8” incision over the knee a hospital stay of 3-5 days and sometimes an additional stay in an inpatient rehabilitation setting before going home. The recovery period(during which the patient walks with a walker or cane) typically lasting from one to three months. The large majority of patients report substantial or complete relief of their arthritic symptoms once they have recovered from a total knee replacement.
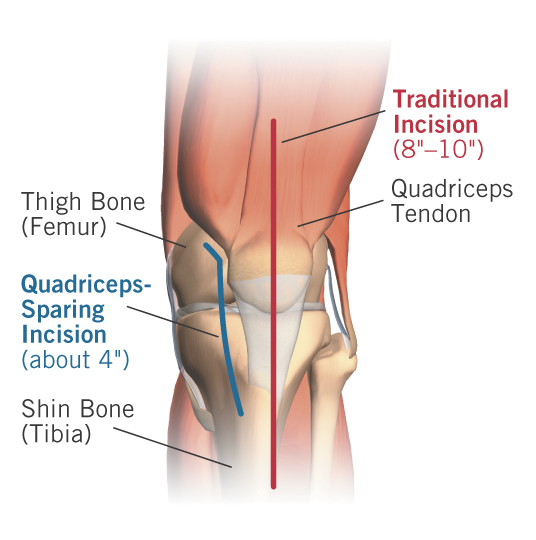
Minimally-invasive quadriceps-sparing total knee replacement is a new surgical technique that allows surgeons to insert the same time-tested reliable knee replacement implants through a shorter incision using surgical approach that avoids trauma to the quadriceps muscle (see figure 1) which is the most important muscle group around the knee. This new technique which is sometimes called quadriceps-sparing knee replacement uses an incision that is typically only 3-4” in length (see figure 2) and the recovery time is much quicker – often permitting patients to walk with a cane within a couple of weeks of surgery or even earlier. The less-traumatic nature of the surgical approach also may decrease post-operative pain and diminish the need for rehab and therapy compared to more traditional approaches.
The main potential benefits of this new technique include:
- More rapid return of knee function. Patients who undergo this procedure seem to get muscle strength and control back more quickly than patients who have had traditional total knee replacement. (See Video) This is because the quadriceps muscle and tendon are not divided in the course of the surgical exposure like in traditional knee replacement and the kneecap is not everted (flipped out of the way) as it is in traditional total knee replacement.
- Smaller incision. While this procedure would not be worth performing for cosmetic benefits many patients do prefer the shorter incision. Traditional knee replacement incisions often measure 8” or longer; minimally-invasive quadriceps-sparing knee replacement incisions are about 4” in length for most patients.
- Decreased post-operative pain. (See Video)This may be a function of the smaller incision and the fact that the incision stays out of the important quadriceps muscle/tendon group.
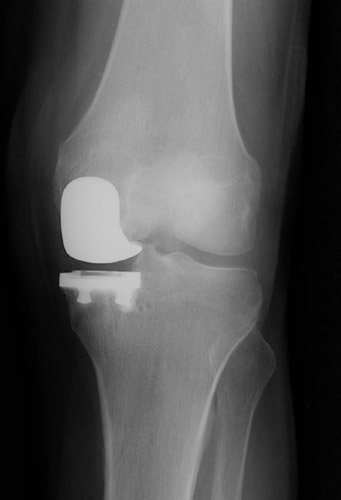
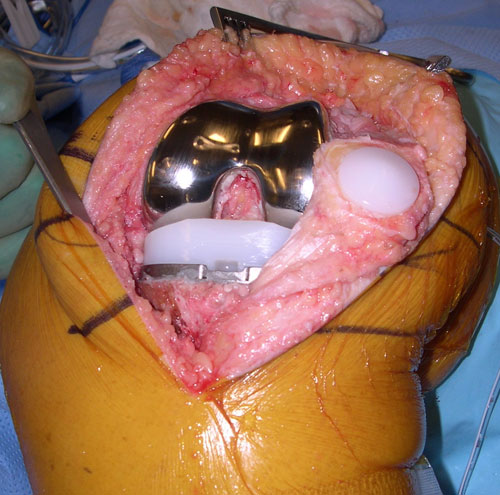
- Same reliable surgical implants as Traditional Knee Replacement. Much has been learned about implant design in the nearly 40-year history of contemporary knee replacement. Minimally-invasive quadriceps-sparing total knee replacement is an evolution of surgical technique which permits the use of time-tested implant designs (see figures 3 and 4). This gives some reassurance that while the surgical approach is new the implants themselves have a good proven track record.
The major apparent risks of the procedure compared to traditional total knee replacement:
- The procedure is new. Though surgeons have studied the approach the studies are recent and have replicated (repeated and verified) by only a few groups of surgeon-scientists. These studies give some insight into which patients and patterns of arthritis are most suitable for this procedure the relative novelty of the approach it is likely that as time passes we will discover more about the risks and shortcomings of this technique. Also even an experienced knee replacement surgeon will have performed many more surgeries through the traditional approach than through the less-invasive method; we know that the more procedures one does the more reliable the results are.
- The procedure is more challenging. Operating through a smaller surgical window takes some getting used to and this can increase operative time compared to procedures performed using the traditional technique. This may increase the likelihood that an intra-operative injury to tendon or ligament might occur which could compromise the result. This may also increase the likelihood of component malalignments which could affect function and durability. However two preliminary studies on this technique in fact found that these adverse outcomes did not take place.
For some patients an implant other than a total knee replacement may be a reasonable choice. Partial knee replacements sometimes called unicompartmental (partial) knee replacements (see figures 5 and 6) also have a long track record in this country and in Europe. Partial knee replacements have been around for decades and offer excellent clinical results just like total knee replacements. Less invasive techniques are available to insert these smaller implants as well but only a minority of knee replacement patients (about 10%) are good candidates for this procedure. Minimally-invasive partial knee replacement (mini knee) is the topic of another article on this website.
By contrast the minimally-invasive quadriceps-sparing total knee replacement is appropriate for most patterns of knee arthritis.
Figure 2 - The skin incision for minimally-invasive quadriceps-sparing total knee replacement is typically about 4? in length compared to about 8? or more for traditional total knee replacements.
Figure 6 - Model of a partial knee replacement. This smaller implant leaves undamaged cartilage in other parts of the knee intact.
Watch Videos
Symptoms & Diagnosis
Characteristics of knee arthritis
There are over 100 types of arthritis and all of them can affect the knee and the knee is the most-commonly affected joint. Most patients who have arthritis are over age 50 but certain types and patterns of arthritis can affect younger patients. Arthritis of the knee causes pain stiffness and sometimes swelling. Patients with more advanced arthritis find that even simple daily activities like walking arising from a chair and performing self-care can be affected. Most patients with arthritis can achieve some measure of relief from activity modifications pills or joint injections; however for some patients these remedies are insufficient to provide a satisfactory quality of life. These patients sometimes consider knee replacement surgery. More details about the common characteristics of knee arthritis follow below:
Pain
Pain is the most noticeable symptom of knee arthritis. In most patients the pain gradually gets worse over time but sometimes has more sudden “flares” where the symptoms get acutely severe. The pain is almost always worsened by weight-bearing and activity. In some patients the pain becomes severe enough to limit even routine daily activities.
Stiffness
Morning stiffness is present in certain types of arthritis; patients with this symptom may notice some improvement in knee flexibility over the course of the day. For information about other kinds of arthritis see our articles on knee arthritis.
Swelling and warmth
Patients with arthritis sometimes will notice these symptoms. If the swelling and warmth are excessive and are associated with severe pain inability to bend the knee and difficulty with weight-bearing those signs might represent an infection. Such severe symptoms require immediate medical attention. Joint infection of the knee is discussed below.
Location
The knee joint has three “compartments” that can be involved with arthritis (see figure 7). Most patients have both symptoms and findings on X-rays that suggest involvement of two or more of these compartments--for example pain on the lateral side (see figure 8) and beneath the kneecap (see figure 9). Patients who have arthritis in two or all three compartments and who decide to get surgery most often will undergo total knee replacement (see figure 10).
However some patients have arthritis limited to one compartment of the knee--most commonly the medial side (see figure 11). When patients with one-compartment arthritis (also called “unicompartmental” arthritis) decide to get surgery they may be candidates for minimally-invasive partial knee replacement (mini knee) (see figure 12).
Types
Inflammatory arthritis
This broad category includes a wide variety of diagnoses including Rheumatoid arthritis, lupus, gout and many others. It is important that patients with these conditions be followed by a qualified rheumatologist as there are a number of exciting new treatments that may decrease the symptoms and perhaps even slow the progression of the joint damage.
Patients with inflammatory arthritis of the knee usually have joint damage in all three compartments and therefore are not good candidates for partial knee replacement. However inflammatory arthritis patients who decide to have total knee replacement have an extremely high likelihood of success; these patients often experience total or near-total pain relief following a well-performed joint replacement.
Osteoarthritis
Osteoarthritis is also called OA or “degenerative joint disease.” OA patients represent the large majority of arthritis sufferers. OA may affect multiple joints or it may be localized to the involved knee. Activity limitations due to pain are the hallmarks of this disease.
OA patients who have symptoms limited to one compartment of the knee sometimes are good candidates for minimally-invasive partial knee replacement (mini knee).
Similar conditions
Meniscus tear
Sometimes patients with knee pain don't have arthritis at all. Each knee has two rings of cartilage called "menisci" (this is the plural form of "meniscus"). The menisci work similarly to shock absorbers in a car.
Menisci may be torn acutely in a fall or as the result of other trauma or they may develop degenerative tears from wear-and-tear over many years. Patients with meniscus tears experience pain along the inside or outside of the knee; sometimes the pain is worse with deep squatting or twisting. Popping and locking of the knee are also occasional symptoms of meniscus tears.
Since some of these symptoms may be present with arthritis and the treatment of arthritis is different from that of meniscus tears it is important to make the correct diagnosis. A good orthopedic surgeon can distinguish the two conditions by taking a thorough history performing a careful physical examination and by obtaining imaging tests. X-rays and Magnetic Resonance Imaging (MRI) scans may be helpful in distinguishing these two conditions.
Joint infections
Also called infectious arthritis or septic arthritis a joint infection is a severe problem that requires emergent medical (and often surgical) attention. If not treated promptly knee infections can cause rapid destruction of the joint; in the worst cases they can become life-threatening.
Symptoms of a knee joint infection include:
- severe pain
- joint swelling and warmth
- fevers and
- marked inability to walk bend the knee or bear weight.
Patients who suffer from arthritis are not more likely to develop such infections. They may occur in anyone. Arthritis patients who develop such infections would notice a significant worsening in their pain as well as some of the other symptoms listed above.
A physician will make the diagnosis of a joint infection based on history and physical examination blood tests and by sampling joint fluid from the knee.
Again a joint infection is a serious condition that requires immediate medical attention.
Incidence and risk factors
Knee involvement by rheumatoid arthritis (RA) is common. Approximately 20-30% of patients with RA will have knees affected by this disease.
Diagnosis
History and physical examination
An orthopedic surgeon will begin the evaluation with a thorough history and physical exam. Based on the results of these steps (s)he may order plain X-rays.
X-rays
If a patient has arthritis of the knee it will be evident on routine X-rays of the joint. X-rays taken with the patient standing up are more helpful than those taken lying down as the way the knee joint functions under load (i.e. standing) provides important treatment clues to the physician.
Also plain X-rays will allow an orthopedic surgeon to determine whether the arthritis pattern would be suitable for total knee replacement or for a different operation such as minimally-invasive partial knee replacement (mini knee).
Treatments
Medications
It is important to distinguish broadly between two types of arthritis: inflammatory arthritis (including Rheumatoid arthritis, lupus and others) and non-inflammatory arthritis (such as osteoarthritis).
Although there is some level of inflammation present in all types of arthritis conditions that fall into the category of true inflammatory arthritis are often very well managed with a variety of medications and more treatments are coming out all the time. Individuals with rheumatoid arthritis and related conditions need to be evaluated and followed by a physician who specializes in those kinds of treatments called a rheumatologist. Excellent non-surgical treatments (including many new and effective drugs) are available for these patients; those treatments can delay (or avoid) the need for surgery and also help prevent the disease from affecting other joints.
So-called non-inflammatory conditions including osteoarthritis (sometimes called degenerative joint disease) also sometimes respond to oral medications (either painkillers like Tylenol or non-steroidal anti-inflammatory drugs like aspirin ibuprofen celebrex or vioxx) but in many cases symptoms persist despite that type of treatment.
It is important to avoid using narcotics (such as Tylenol #3 vicoden percocet or oxycodone) since they are have many side effects are habit-forming and make it harder to achieve pain-control safely and effectively after surgery should that become necessary. Narcotics are designed for people with short-term pain (like after a car accident or surgery) or for people with chronic pain who are not surgical candidates. People who feel they need narcotics to achieve pain control should consider seeing a joint replacement surgeon (an orthopedic surgeon with experience in knee replacements) to see whether surgery is a better option.
Nutritional supplements like glucosamine and chondroitin have been shown to decrease pain in many patients who use them. These products typically take 6-8 weeks to achieve their maximum effect. However they do not work for all patients who try them and despite what some advertisements suggest they do not appear to regrow cartilage or reverse the arthritic process.
Joint injections either with corticosteroids (“cortisone shots”) or with viscosupplements like Synvisc or Hyalgan may also provide temporary relief. These products do not work in all people who try them and there is some risk of infection associated with injecting the knee joint though this is not very likely.
Exercises
There is little evidence to suggest that knee arthritis can be prevented or caused by exercises or activities unless the knee was injured (or was otherwise abnormal) before the exercise program began. There is no evidence that once arthritis is present in a knee joint any exercises will alter its course.
However exercise and general physical fitness have numerous other health benefits. Regular range of motion exercises and weight bearing activity are important in maintaining muscle strength and overall aerobic (heart and lung) capacity and help prevent the development of osteoporosis which can complicate later treatment. Certainly people who are physically fit are more resilient and in general are more able to overcome the problems associated with arthritis. Physically fit people also tend to recover more quickly from surgery should that eventually be necessary to treat the knee arthritis.
Possible benefits of minimally-invasive (quadriceps-sparing) total knee replacement
Regardless of whether a traditional total knee replacement or a minimally-invasive (quadriceps-sparing) total knee replacement is performed the goals and possible benefits are the same: relief of pain and restoration of function.
The large majority (more than 90 percent) of total knee replacement patients experience substantial or complete relief of pain once they have recovered from the procedure. The large majority walk without a limp and most don’t require a cane even if they used one before the surgery. It is quite likely that you know someone with a knee replacement who walks so well that you don’t know (s)he even had surgery! Frequently the stiffness from arthritis also is relieved by the surgery. Very often the distance one can walk will improve as well because of diminished pain and stiffness. The enjoyment of reasonable recreational activities such as golf dancing traveling and swimming almost always improves following total knee replacement.
However there are some potential benefits of the newer less-invasive total knee technique over the traditional technique of total knee replacement.
The main potential benefits of this new technique include:
- More rapid return of knee function. Patients who undergo this procedure seem to get muscle strength and control back more quickly than patients who have had traditional total knee replacement. This is because the quadriceps muscle and tendon are not divided in the course of the surgical exposure like in traditional knee replacement and the kneecap is not everted (flipped out of the way) as it is in traditional total knee replacement.
- Smaller incision. While this procedure would not be worth performing for cosmetic benefits many patients do prefer the shorter incision. Traditional knee replacement incisions often measure 8” or longer; minimally-invasive quadriceps-sparing knee replacement incisions are about 4” in length for most patients.
- Decreased post-operative pain. This may be a function of the smaller incision and the fact that the incision stays out of the important quadriceps muscle/tendon group.
- Same reliable surgical implants as Traditional Knee Replacement. Much has been learned about implant design in the nearly 40-year history of contemporary knee replacement. Minimally-invasive quadriceps-sparing total knee replacement is an evolution of surgical technique which permits the use of time-tested implant designs. This gives some reassurance that while the surgical approach is new the implants themselves have a good proven track record.
Joint replacement surgery is the most effective method for restoring comfort and function to knees damaged by severe arthritis. When the normally smooth surfaces of the knee joint are severely damaged by arthritis injury or surgery total knee replacement may be the most effective method for restoring comfort and function to the joint. For a minority of patients with arthritis a minimally-invasive partial knee replacement is an option instead of total knee replacement but most patients with knee arthritis who undergo surgery are better served with total knee replacement.
Other surgical options such as arthroscopy or “clean up” operations have not been shown to give lasting benefit.
Knee fusion can stabilize the joint and decrease pain but does not allow motion at the knee joint.
For selected younger and more active patients realigning the joint using a procedure called osteotomy may be appropriate; however the durability and pain relief of this procedure does not seem to measure up to joint replacement particularly in older patients.
Who should consider minimally-invasive (quadriceps-sparing) total knee replacement?
Joint replacement surgery is considered when:
- the arthritis is a major problem for the patient
- the patient is sufficiently healthy to undergo the procedure
- the patient understands and accepts the risks and alternatives
- there is sufficient bone and tendon to permit the surgery and
- the surgeon is experienced in knee replacement surgery.
What happens without surgery?
Arthritis is often progressive and symptoms typically get worse over time. In some patients the symptoms wax and wane causing “good days and bad days.” Knee arthritis does not usually improve on its own.
Surgical options
If a knee surgeon and a patient decide that non-operative treatments have failed to provide significant or lasting relief there are sometimes different operations to choose from.
Total knee replacement
Long considered the “gold standard” operation for knee arthritis total knee replacement is still by far the most commonly-performed joint replacement procedure (see figure 13). It is most suitable for middle-aged and older people who have arthritis in more than one compartment of the knee (see figures 14 and 15) and who do not intend to return to high-impact athletics or heavy labor. Results of this procedure generally are excellent with 90-95% of total knee replacements continuing to function well more than 10 years after surgery.
There are now several ways to perform total knee arthroplasty:
Minimally-Invasive Quadriceps-Sparing Total Knee Replacement
This is a new technique that permits insertion of the joint replacement implants through a short incision – typically about 4” in length – and allows the surgeon to do so without disturbing the quadriceps muscle or tendon. The shorter incision but more importantly the avoidance of the quadriceps muscle and tendon may result in less pain a quicker rehabilitation and earlier restoration of function. However this procedure may not be appropriate for all patients with knee arthritis who undergo knee replacement; patients who are heavier have osteoporosis in addition to arthritis and who have significant joint deformity or stiffness may be better served with traditional approaches to total knee replacement.
Traditional Total Knee Replacement
The joint replacement in inserted using an incision that typically measures 8”-10” in length over the front of the knee. The quadriceps tendon and/or muscle is entered and the kneecap is moved out of the way to permit the surgeon to see the inside of the knee fully and clearly. Restoring range of motion and quadriceps strength is the biggest part of the patient’s rehabilitation after the surgery. This approach has been used for over three decades with excellent results. It is adaptable and permits surgeons to perform the procedure in patients who are heavy who have joint deformity or who have severe stiffness.
But not every patient with knee arthritis needs (or should have) total knee replacement. There are many other surgical options available for patients with certain patterns of knee arthritis. These include:
Minimally-invasive partial knee replacement (unicompartmental knee)
Patients who are of appropriate age--certainly older than age 40 and older is better--and who have osteoarthritis limited to one compartment of the knee may be candidates for an exciting new surgical technique minimally-invasive partial knee replacement (mini knee) (see figures 16 17 and 18). Partial knee replacements have been done for over 20 years and the “track record” on the devices used for this operation is excellent. The new surgical approach which uses a much smaller incision than traditional total knee replacement significantly decreases the amount of post-operative pain and shortens the rehabilitation period. The decision of whether this procedure is appropriate for a specific patient can only be made in consultation with a skillful orthopedic surgeon who is experienced in all techniques of knee replacement.
Minimally-invasive partial knee replacement (mini knee) is not for everyone. Only certain patterns of knee arthritis are appropriately treated with this device through the smaller approach.
Generally speaking patients with inflammatory arthritis (like Rheumatoid arthritis or lupus) and patients with diffuse arthritis all throughout the knee should not receive partial knee replacements.
Patients who are considering knee replacements should ask their surgeon whether minimally-invasive partial knee replacement (mini knee) is right for them.
Knee arthroscopy
If X-rays don’t show very much arthritis and the surgeon suspects (or has identified by MRI) a torn meniscus knee arthroscopy may be a good choice. This is a relatively minor procedure that is usually done as an outpatient and the recovery is fairly quick in most patients.
However if X-rays demonstrate a significant amount of arthritis this may not be a good choice. Knee arthroscopy for arthritis fails to relieve pain in about half of the patients who try it.
Osteotomy
For younger patients (typically under age 40 but this age cutoff is flexible) who desire to return to a high level of athletic activity or physical work a procedure called osteotomy (which means “cutting the bone”) might be worth considering. This option is suitable only if the arthritis is limited to one compartment of the knee (for more information about arthritis in one compartment of the knee see the "Location" section on Symptoms & Diagnosis of this article).
Osteotomy involves cutting and repositioning one of the bones around the knee joint. This is done to re-orient the loads that occur with normal walking and running so that these loads pass through a non-arthritic portion of the knee. That’s why it doesn’t work well if more than one compartment of the knee is involved--in those patients there is no “good” place through which the load can be redistributed.
Knee fusion
Knee fusion also called “arthrodesis ” permanently links the femur (thigh bone) with the tibia (shin bone) creating one long bone from the hip to the ankle. It removes all motion from the knee resulting in a stiff-legged gait.
Because there are so many operations that preserve motion this older procedure is seldom performed as a first-line option for patients with knee arthritis. It is sometimes used for severe infections of the knee certain tumors and patients who are too young for joint replacement but are otherwise poor candidates for osteotomy.
Watch videos:
Effectiveness
Current evidence suggests that when total knee replacements are done well in properly selected patients success is achieved in the large majority of patients and the implant serves the patient well for many years.
Many studies show that 90-95 percent of total knee replacements are still functioning well 10 years after the surgery. Most patients walk without a cane most can do stairs and arise from chairs normally and most resume their desired level of recreational activity.
The goal of minimally-invasive quadriceps-sparing total knee replacement is to capitalize on the decades of experience surgeons have gained in total knee implant design and intra-operative ligament balancing but provide patients with a faster recovery and less post-operative pain. The same knee replacement implants and materials are used the point of attachment to the bones is the same (bone cement) and the same attention to surgical detail limb alignment and ligament balancing are given during the newer less-invasive procedure as during the traditional approach. It is important to remember that this is a new procedure compared to traditional total knee replacement and as a result we do not have long-term follow-up on outcomes. However short term studies on knee component and limb alignment and peri-operative complications have found results with those endpoints that are comparable to traditional approaches while providing patients with faster rehabilitation.
Regardless of the technique used to insert the knee replacement (traditional or minimally-invasive) in the event that a total knee replacement requires re-operation sometime in the future it almost always can be revised (re-done) successfully. However results of revision knee replacement are typically not as good as first-time knee replacements.
There is good evidence that the experience of the surgeon correlates with outcome in total knee replacement surgery; for this reason it is best to have the initial surgery done by an individual who is experienced (fellowship-trained and with a practice that focuses on knee replacement) in this kind of work.
Likewise the new technique of minimally-invasive quadriceps sparing knee replacement should only be performed by surgeons who have taken special training on the instruments and surgical approaches and who have experience using less-invasive surgical techniques around the knee.
Surgeons with this level of experience have been shown to have fewer complications and better results than surgeons who haven’t done as many knee replacements. It is therefore important that the surgeon performing the technique be not just a good orthopedic surgeon but a specialist in knee replacement surgery and in less-invasive joint replacement.
Urgency
Total knee replacement is elective surgery. With few exceptions it does not need to be done urgently and can be scheduled around important life-events. This does not change regardless of the technique used (minimally-invasive or traditional).
Risks
Like any major surgical procedure total knee replacement is associated with certain medical and surgical risks. Although major complications are uncommon they may occur; the possibilities include blood clots bleeding and anesthesia-related or medical risks such as cardiac risks stroke and in rare instances (large studies have calculated the risk to be less than 1 in 400) death.
Risks specific to knee replacement include infection (which may result in the need for more surgery) nerve injury the possibility that the knee may become either too stiff or too unstable to enjoy it a chance that pain might persist (or new pains might arise) and the chance that the joint replacement might not last the patient's lifetime or might require further surgery.
Minimally-invasive quadriceps-sparing total knee replacement is a new procedure. For this reason it is fair to say that the specialty will need to pay close attention to results to make sure they are as good or better than the traditional techniques that have been in common use for quite some time now. However preliminary studies on the technique have shown no increases in surgical or medical risk with this approach compared to traditional total knee arthroplasty and these same studies have shown benefits in terms of post-operative pain and early recuperation and rehabilitation after surgery.
While the overall list of complications may seem long and intimidating the overall frequency of major complications following total knee replacement is low usually less than 5 percent (one in 20). Obviously the overall risk of surgery is dependent both on the complexity of the knee problem but also on the patient's overall medical health.
The major apparent risks of the minimally-invasive quadriceps-sparing procedure compared to traditional total knee replacement include the following:
- The procedure is new. Though surgeons have studied the approach the studies are recent and have replicated (repeated and verified) by only a few groups of surgeon-scientists. These studies give some insight into which patients and patterns of arthritis are most suitable for this procedure the relative novelty of the approach it is likely that as time passes we will discover more about the risks and shortcomings of this technique. Also even an experienced knee replacement surgeon will have performed many more surgeries through the traditional approach than through the less-invasive method; we know that the more procedures one does the more reliable the results are.
- The procedure is more challenging. Operating through a smaller surgical window takes some getting used to and this can increase operative time compared to procedures performed using the traditional technique. This may increase the likelihood that an intra-operative injury to tendon or ligament might occur which could compromise the result. This may also increase the likelihood of component malalignments which could affect function and durability. However two preliminary studies on this technique in fact found that these adverse outcomes did not take place.
Managing risk
Many of the major problems that can occur following traditional or minimally-invasive total knee replacement can be treated. The best treatment though is prevention. An orthopedic surgeon will use antibiotics before during and after surgery to minimize the likelihood of infection. (S)he will take steps to decrease the likelihood of blood clots such as early patient mobilization and use of blood-thinning medications in some patients. Patients are evaluated by a good internist and/or anesthesia provider in advance of the surgery in order to decrease the likelihood of a medical or anesthesia-related complication. Good surgical technique can help minimize the knee-specific risks--so choosing a fellowship-trained and experienced knee replacement surgeon is important.
Again the overall likelihood of a severe complication is typically less than 5 percent when such steps are taken.
Preparation
Patients undergoing total knee replacement surgery usually will undergo a pre-operative surgical risk assessment. When necessary further evaluation will be performed by an internal medicine physician who specializes in pre-operative evaluation and risk-factor modification. Some patients will also be evaluated by an anesthesiologist in advance of the surgery.
Routine blood tests are performed on all pre-operative patients; chest X-rays and electrocardiograms are obtained in patients who meet certain age and health criteria as well.
Before a scheduled surgery, some people choose to 'bank' their own blood to be used during their recovery. While this can offer peace of mind and minimize the need for donor blood, it isn't the right choice for everyone. We look at each patient’s health history and the specific details of their upcoming surgery to decide if predonating is the safest and most helpful path forward.
Surgeons will often spend time with the patient in advance of the surgery making certain that all the patient's questions and concerns as well as those of the family are answered.
Timing
The decision to have minimally-invasive or traditional total knee replacement is a quality of life choice best made by an educated patient in consultation with an experienced surgeon. The timing of this procedure should revolve around the patient’s medical condition and social support networks. Only rarely does knee replacement get done as an urgent procedure. Very occasionally in cases of rheumatoid or other types of inflammatory arthritis excessive delays can result in the loss of bone and tendon tissue. These losses can compromise the quality of the surgery and its result.
Costs
The surgeon's office should provide a reasonable estimate of:
- the surgeon's fee
- the hospital fee and
- the degree to which these should be covered by the patient's insurance.
Surgical team
Minimally-invasive quadriceps-sparing total knee replacement requires an experienced orthopedic surgeon and the resources of a large medical center. Patients should inquire as to the number of knee arthroplasty procedures that the surgeon performs each year overall and how many minimally-invasive knee replacements the surgeon has performed.
Some patients have complex medical needs and around surgery often require immediate access to multiple medical and surgical specialties and in-house medical physical therapy and social support services.
Finding an experienced surgeon
There is good evidence that the experience of the surgeon performing partial knee replacement affects the outcome. It is important that the surgeon be experienced--and preferably fellowship-trained--knee replacement surgeon.
Some questions to consider asking your knee surgeon:
- Are you board certified in orthopedic surgery?
- Have you done a fellowship (a year of additional training beyond the five years required to become an orthopedic surgeon) in joint replacement surgery?
- How many knee replacements do you do each year?
- How many minimally-invasive knee replacements have you performed?
Facilities
A large hospital usually with academic affiliation and equipped with state-of-the-art radiologic imaging equipment and medical intensive care unit is clearly preferable in the care of patients with knee arthritis. These centers have surgical teams and facilities specially designed for this type of surgery. They also have nurses and therapists who are accustomed to assisting patients in their recover from knee replacement surgery.
Technical details
Minimally-invasive quadriceps-sparing total knee replacement surgery begins by performing a sterile preparation of the skin over the knee to prevent infection followed by inflation of a tourniquet to prevent blood loss during the operation.
Next a well-positioned skin incision – typically about 4” in length (see figure 19) though this varies with the patient’s size – is made down the front of the knee just adjacent to the kneecap and the knee joint is inspected and preliminary ligament balancing is performed.
Next specially-designed alignment rods and cutting jigs – which are smaller and easier to pass through the smaller incision than those used for traditional total knee replacement – are used to remove enough bone from the end of the femur (thigh bone) the top of the tibia (shin bone) and the underside of the patella (kneecap) to allow placement of the joint replacement implants. Proper sizing and alignment of the implants as well as final balancing of the knee ligaments all are critical for normal post-operative function and good pain relief. Again these steps are complex and considerable experience in minimally-invasive knee replacement is required in order to make sure they are done reliably case after case. Provisional (trial) implant components are placed without bone cement to make sure they fit well against the bones and are well aligned; at this time good function--including full flexion (bend) extension (straightening) and ligament balance--is verified.
Finally the bone is cleaned using saline solution and the joint replacement components are cemented into place using polymethylmethacrylate bone cement (see figure 20). The surgical incision is closed using stitches and staples.
Anesthetic
Total knee replacement may be performed under epidural spinal or general anesthesia. We usually prefer epidural or spinal anesthesia since these can help provide pain relief in the days following surgery and allow faster more comfortable progress in physical therapy.
Length of minimally-invasive (quadriceps-sparing) total knee replacement
No two knee replacements are alike and there is some variability in operative times but a typical total knee replacement takes about 60-80 minutes to perform when traditional techniques are used because the wider exposure permits more rapid progress through the technical steps of the procedure (see Figure 21).
Pain and pain management
Whenever possible we use a spinal anesthetic with a long-acting morphine product to provide pain relief for up to 24 hours after surgery. Beyond that pain medications by vein or in pill form are used to permit early rapid rehabilitation.
Alternatively an epidural catheter (a very thin flexible tube placed into the lower back at the time of surgery) to manage post-operative discomfort. This device is similar to the one that is used to help women deliver babies more comfortably. As long as the epidural is providing good pain control we leave it in place for two days after surgery. After the epidural is removed pain pills usually provide satisfactory pain control. Patients who have epidural or spinal anesthesia can expect to walk with crutches or a walker and to take the knee through a near-full range of motion starting on the day after surgery. In the days that follow the patient is transitioned on to pain pills to allow rehabilitation and rapid recovery following minimally-invasive quadriceps-sparing total knee replacement.
Some patients are not candidates for spinal or epidural anesthetics or choose not to have them. These patients receive pain medications by vein for the first day or two and then can go home on pain pills following minimally-invasive quadriceps-sparing total knee replacement.
Use of medications
Following discharge from the hospital most patients will take oral pain medications--usually Percocet Vicoden or Tylenol #3--for one to three weeks after the procedure mainly to help with physical therapy and home exercises for the knee.
Aggressive rehabilitation is desirable following this procedure and a high level of patient motivation is important in order to get the best possible result. “Minimally-invasive” does not mean “non-invasive” or “minor”; it is important to realize that even with the newer technique the biggest key to recovery is a motivated patient who is diligent about his/her rehabilitation and home exercises. Pushing through a certain amount of discomfort or pain is part of recovery from any knee replacement.
Oral pain medications help this process in the weeks following the surgery.
Most patients take some narcotic pain medication for between 2 and 6 weeks after surgery. Patients should not drive while taking these kinds of medications.
Effectiveness of medications
While any surgical procedure is associated with post-operative discomfort most patients who have had the total knee replacements say that the pain is very manageable with the pain medications and the large majority look back on the experience and find that the pain relief given by knee replacement is well worth the discomfort that follows this kind of surgery.
Minimally-invasive quadriceps-sparing total knee replacement seems to be associated with less pain than traditional total knee replacement. However it is important to realize that it is a real surgical procedure and a good outcome depends on a motivated patients who is willing to push through a certain amount of discomfort to get the best possible knee motion and outcome after surgery.
Important side effects
Pain medications can cause drowsiness slowness of breathing difficulties in emptying the bladder and bowel nausea vomiting and allergic reactions. Patients who have taken substantial narcotic medications in the recent past may find that usual doses of pain medication are less effective. For some patients balancing the benefit and the side effects of pain medication is challenging. Patients should notify their surgeon if they have had previous difficulties with pain medication or pain control.
Hospital stay
The average hospital stay after traditional total knee replacement is three days and most patients spend several more days in an inpatient rehabilitation facility. Patients who prefer not to have inpatient rehabilitation may spend an extra day or two in the hospital before discharge to home.
The overall duration of hospitalization after minimally-invasive quadriceps-sparing total knee replacement typically is 48 hours; some patients need to stay for a third day but many do not. Patients generally are discharged directly home from the hospital after minimally-invasive quadriceps-sparing total knee replacement and don't require any inpatient rehabilitation. Ultimately the length of hospital stay is individualized to meet each patient’s needs and discharge occurs when the patient can perform the necessary range of motion exercises and when home support systems for the patient are in place.
Recovery and rehabilitation in the hospital
Patients begin range-of-motion exercises on the day following surgery. Patients are encouraged to sit stand and walk as much as possible in the days following the procedure. Patients who regain good range-of-motion early (defined as near-full extension and bend beyond 90 degrees in the first day or two after surgery) typically do very well so this is emphasized in physical therapy sessions that take place twice daily after surgery. Most patients begin with a walker or crutches and transition to a cane is encouraged and permitted as soon as patients tolerate it provided their balance is good. Therapists instruct all patients in how to perform a home exercise program to allow recovery to continue after discharge.
Sample videos
- Video: Ten days after quad sparing total knee replacement walking without a cane. (1.50 MB)
- Video: In recovery 30 minutes after MIS total knee replacement. (3.76 MB)
- Video: Patient skiing after Total Knee Replacement
Hospital discharge
The average hospital stay after minimally-invasive total knee replacement is two days with some patients staying three. Patients generally are discharged to their homes directly from the hospital (again usually after a 48-hour stay) and generally do not require inpatient rehabilitation. Sometimes the stay is even shorter.
At the time of discharge the patient should be relatively comfortable on oral medications should have a dry incision should understand their exercises and should feel comfortable with the plans for managing the knee. Management of these limitations requires advance planning to accomplish the activities of daily living during the period of recovery.
Convalescent assistance
Most patients will go home following their hospital stay. Home physical therapy typically 3 times per week is initiated as soon as possible following hospital discharge.
Patients are encouraged to walk as normally as possible immediately following minimally-invasive quadriceps-sparing total knee replacements. Most people use crutches or a walker for a week and then a cane for another week or so beyond that. Most people are walking nicely by about two weeks after surgery (see video above).
Patients are allowed to shower as soon as the surgical incision has been dry for a day or so.
Patients should not resume driving until they feel their reflexes are completely normal and until they feel they can manipulate the control pedals of the vehicle without guarding from knee discomfort. Certainly patients should not drive while taking narcotic-based pain medications. On average patients are able to drive between three and six weeks after the surgery.
Physical therapy
The length of physical therapy varies based upon patient age fitness and level of motivation but usually lasts for about four weeks. Two to three therapy sessions per week are average for this procedure. Sometimes even less therapy is needed; occasionally a bit more.
Can rehabilitation be done at home?
All patients are given a set of home exercises to do between supervised physical therapy sessions and the home exercises make up an important part of the recovery process. However supervised therapy--which is best done in an outpatient physical therapy studio--is extremely helpful and those patients who are able to attend outpatient therapy are encouraged to do so.
For patients who are unable to attend outpatient physical therapy home physical therapy is arranged.
Usual response
No two patients are alike and recovery varies somewhat based on the complexity of the knee reconstruction and the patient’s health fitness and level of motivation.
Most people walk using crutches or a walker for 2 weeks then use a cane for about 2 more weeks.
Most patients obtain and keep at least 90 degrees of motion (bending the knee to a right angle) by a day or two after surgery and most patients ultimately get more than 110 degrees of knee motion.
Most patients can return to sedentary (desk) jobs by about 4 weeks; return to more physical types of employment must be addressed on a case-by-case basis.
Most patients are back to full activities--without the pain they had before surgery--by about two months after the operation.
Risks
This is a safe rehabilitation program with little risk.
Duration of rehabilitation
Once the range of motion and strength goals are achieved the exercise program can be cut back to a minimal level. But maintaining lifelong fitness should be everyone’s goal!
Returning to ordinary daily activities
Most patients are walking unassisted following this procedure by about a two weeks after surgery (see video).
Most patients can return to desk work at least for part days by about a three weeks after surgery.
Sample Video
Long-term patient limitations
The goal of total knee replacement is to return patients to a high level of function without knee pain. The large majority of patients are able to achieve this goal. However since the joint replacement components have no capacity to heal damage from injury sustained after surgery we offer some common-sense guidelines for athletic leisure and workplace activities:
Recommended:
- Swimming
- Water aerobics
- Cross-country skiing or Nordic Track
- Cycling or stationary bike
- Golf
- Dancing
- Sedentary occupations (desk work)
Permitted when the patient finds them comfortable:
- Hiking
- Gentle doubles tennis
- Gentle downhill skiing
- Light labor (jobs that involve driving walking or standing but not heavy lifting)
Not recommended:
- Jogging or running
- Impact exercises
- Sports that require twisting/pivoting (aggressive tennis basketball racquetball)
- Contact sports
- Heavy labor
Since the joint replacement includes a bearing surface which potentially can wear walking or running for fitness are not recommended. Some patients feel well enough to do this and so need to exercise judgment in order to prolong the life-span of the implant materials. Swimming water exercises cycling and cross country skiing (and machines simulating it like Nordic Track) can provide a high level of cardiovascular and muscular fitness without excessive wear on the prosthetic joint materials.
Costs
The surgeon and therapist should provide the information on the usual cost of the rehabilitation program.
Summary of minimally-invasive (quadriceps-sparing) total knee replacement for knee arthritis
Total knee replacement is a reliable surgical technique in which the painful arthritic surfaces of the knee joint are replaced with well-engineered bearing surfaces. Pain is substantially improved and function regained in more than 90% of patients who have the operation.
Minimally-invasive quadriceps-sparing total knee replacement is a new technique for implanting well-tested total knee replacement components while minimizing post-operative pain and the time to full recovery. The length of the surgical incision while not a goal of the procedure is about half as long using the minimally-invasive approach compared to traditional total knee replacement approaches. One needs to remember that this is a new technique and although preliminary studies are promising it is likely we will continue to learn more about this procedure as time passes and there may be risks to this approach that are not fully appreciated at this time.
Like any major procedure there are risks to total knee surgery and the decision to have a knee replacement must be considered a quality-of-life choice that individual patients make with a good understanding of what those risks are.
Knee replacement is a surgical technique that has many variables; like most areas of medicine ongoing research will continue to help the technique evolve. It is important to learn as much as possible about the condition and the treatment options that are available before deciding whether--or how--to have a knee replacement done. While many of the changes now being explored in the field of total knee replacement may eventually be shown to be legitimate advances – perhaps including alternative bearing surfaces – it is important to compare them carefully to traditional total knee replacement performed using well established techniques which we know are 90-95% likely to provide pain relief and good function for more than 10 years after the surgery.