Edited by:
Professor,
UW Orthopaedics & Sports Medicine

Associate Professor,
UW Orthopaedics & Sports Medicine
Last updated: Saturday, March 26, 2011
Follow our shoulder arthritis blog
http://shoulderarthritis.blogspot.com/
On which we try to provide the best and most current information on shoulder arthritis.
To read more about Glenohumeral Arthritis, please visit our online Shoulder Arthritis Book by Dr. Frederick A. Matsen.
Contact
If you have questions regarding the ream and run procedure, feel free to email Frederick A. Matsen III, M.D. at matsen@uw.edu.
What is shoulder arthritis?
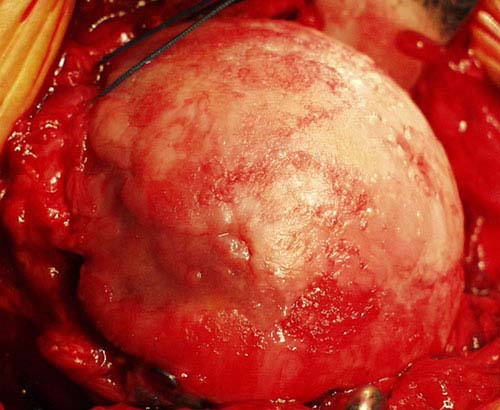
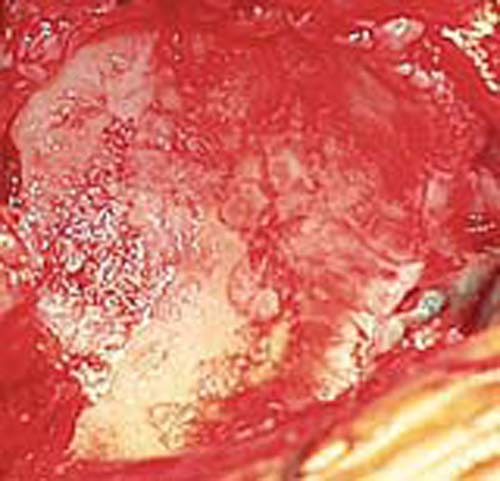
Shoulder arthritis is a condition in which the cartilage that normally provides a smooth covering over the ball and socket is lost. This cartilage loss can result from degeneration, wear and tear, inflammatory disease (i.e. rheumatoid arthritis), injury or prior surgery.
Who usually gets shoulder arthritis?
- When arthritis occurs in a younger person, it is often due to injury or problems from a previous surgery or rheumatoid arthritis.
- When arthritis occurs in an older person, it is usually from wear and tear or from a rotator cuff problem.
What are the symptoms of shoulder arthritis?
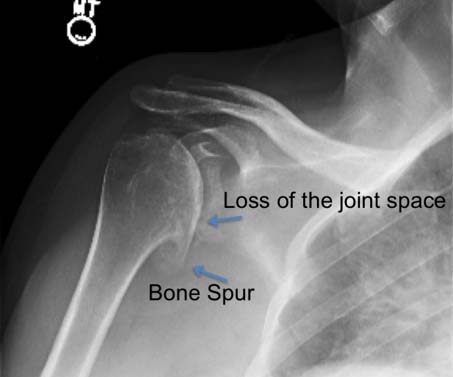
Shoulder arthritis often leads to shoulder pain, weakness, stiffness of the joint, bone spurs and loss of the normal shape of the bones. It may also grind and catch when the shoulder moves. When arthritis is advanced, it may prevent work, play, activities of daily living and comfortable sleep.
What tests show if shoulder arthritis is present?
The best test to show arthritis is a special set of x-rays. The x-ray to the right shows bone spurs and loss of the normal space between the ball (head of the humerus) and socket (glenoid). These are two findings that we look for that demonstrate arthritis in the shoulder.
Shoulder Arthritis Images
What is the treatment for shoulder arthritis?
Mild cases of arthritis of the shoulder can be treated anti-inflammatory medications and with gentle shoulder stretching exercises to maintain the range of motion.
When shoulder arthritis is advanced and does not respond to gentle exercises, consideration is given to joint replacement surgery in which the joint surfaces are replaced, such as with a ‘ream and run’, or a total shoulder arthroplasty may be considered. These procedures are usually very effective in reducing the symptoms of shoulder arthritis. Shoulder joint reconstruction can now be performed with minimal involvement of the deltoid and rotator cuff muscles. Ordinarily gentle and simple rehabilitative exercises are started immediately after surgery and are continued for a year to maximize the recovery of comport, strength, range of motion and function.
When shoulder arthritis is combined with large rotator cuff tear (cuff tear arthropathy), a reverse total shoulder may be considered
What are the risks with surgical treatment?
The risks of shoulder surgery include but are not limited to the following:
- infection,
- injury to nerves and blood vessels,
- fracture,
- stiffness or instability of the joint,
- loosening or wear of the artificial parts,
- failure of the rotator cuff,
- pain, and
- the need for additional surgeries.
There are also risks to anesthesia and blood transfusion (although transfusions are not always necessary). An experienced shoulder joint replacement team that does many such procedures each month will use special techniques to minimize these risks, but cannot totally eliminate them.
Can patients regain all of their shoulder function and how long would it to fully recover after the surgery?
A shoulder replacement can never be as good as a normal shoulder. However, in most cases a technically sound surgery coupled with a good rehabilitative effort on the part of the patient will lead to a major improvement in comfort and function. The first goal of rehabilitation is to restore range of motion. Once this is achieved, the focus shifts to strength and endurance. While improvements may be evident soon after surgery, gains in strength, range, and coordination may continue for up to a year after surgery.
The specific individual rehabilitation program after surgery can only be specified by the surgeon who performed the procedure in view of the specifics of the condition of the shoulder and the procedure performed. It is important that the repaired tendons are not challenged until they have had a chance to heal. Usually the patient is asked to lift nothing heavier than a cup of coffee for six weeks after the surgery; the use of the shoulder is increased progressively after that.
If I need surgery, where should it be done; what is the effect of the surgeon's experience?
On one hand it seems convenient to have surgery done close to home. On the other hand, recent published research has shown that “the patients of surgeons with higher average annual caseloads of total shoulder arthroplasties and hemiarthroplasties have decreased complication rates and hospital lengths of stay compared with the patients of surgeons who perform fewer of these procedures.” (you may wish to read this JBJS article). In this study the surgeons were categorized according to the number of procedures they performed: low-volume surgeons performed an average of 0.29 procedure per year, whereas middle and high-volume surgeons performed an average of 1.6 and 7.54 procedures, per year, respectively. For perspective, the surgical team at the University of Washington performs well over 200 shoulder replacement surgeries per year and has done so for the past two decades. Many of these patients have come from other western states – California, Oregon, Montana, Alaska, Idaho, Wyoming – and some from the mid-west and the east coast.
10 surgery questions for your surgeon before having surgery
For more information, see our Shoulder Arthritis page. If you have questions about surgery for shoulder arthritis, please email us at shoulderarthritis@uw.edu. We will try to answer your questions as soon as possible.