Surgery with a dependable, time-tested conservative prosthesis and accelerated rehabilitation can lessen pain and improve function in shoulders with arthritis
Last updated: January 17, 2014
Edited by:
See: The Shoulder Arthritis Book at
http://shoulderarthritis.blogspot.com/2011/03/what-is-difference-between-shoulder.html
See: The Rotator Cuff Tear Book at
http://shoulderarthritis.blogspot.com/2013/12/the-rotator-cuff-tear-book.html
Overview
Follow our blog
http://shoulderarthritis.blogspot.com/
On which we try to provide the best and most current information on shoulder arthritis.
To read more about Shoulder Arthritis, please visit our online Shoulder Arthritis Book by Dr. Frederick A. Matsen.
Contact
If you have questions regarding total shoulder joint arthroplasty, feel free to email Frederick A. Matsen III, M.D. at matsen@uw.edu.
Click to enlarge
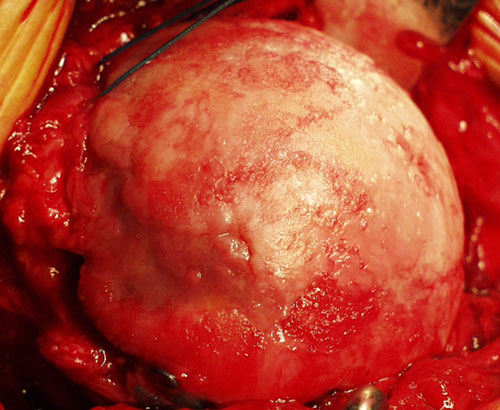
Figure 1 - This is a humeral head
of an arthritic shoulder
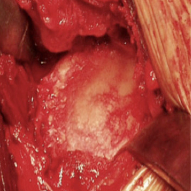
Figure 2 - This is the glenoid socket
of an arthritic shoulder
Figure 3 - Humeral implant
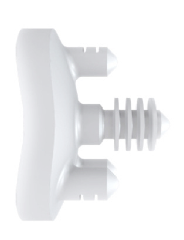
Figure 4 - Glenoid implant
Total shoulder joint replacement surgery (arthroplasty) helps restore comfort and function to shoulders damaged by degenerative joint disease, osteoarthritis, or rheumatoid arthritis.
In shoulder arthritis the joint surface is destroyed by wear and tear, inflammation, injury, or previous surgery. Figure 1 shows the surface of a ball of the shoulder joint (humeral head) that has been destroyed by arthritis. Figure 2 shows the corresponding surface of the glenoid socket. This joint destruction makes the shoulder stiff, painful and unable to carry out its normal functions.
Treatment of shoulder arthritis may include exercises, a ream and run procedure, a total shoulder, or in special cases, a reverse total shoulder.
The goal of shoulder replacement arthroplasty is to restore the best possible function to the joint by removing scar tissue, balancing muscles, and replacing the destroyed joint surfaces with artificial ones. The damaged humeral head is replaced with a metal prosthesis fixed in the shaft of the arm bone (Figure 3) and the damaged glenoid socket is resurfaced with a high-density polyethylene prosthesis (Figure 4).
The diagnosis of shoulder arthritis is made from a history and physical examination and from properly taken x-rays of the shoulder (Figure 5). The characteristic findings of osteoarthritis are shown on figures 6 and 7.
After performing a clinical exam and x-rays (see figure named "X-rays" on the right), a shoulder surgeon experienced in joint replacement can find out if arthritis is the cause of the problem and if surgery would be helpful. Patients are most likely to benefit from this surgery if they are well motivated and in good health.
The goal of shoulder replacement arthroplasty is to restore the best possible function to the joint by removing scar tissue, balancing muscles, and replacing the destroyed joint surfaces with artificial ones.
Total shoulder joint replacement arthroplasty is a highly technical procedure and is best performed by a surgical team who performs this surgery often. Such a team can maximize the benefit and minimize the risks.
If you have questions about this procedure, please feel free to email Dr. Matsen at matsen@uw.edu.
used to diagnose arthritis
of an arthritic shoulder

of an arthritic shoulder

Streaming video
Dr. Matsen and Sarah Jackins, physical therapist with the UW Bone and Joint Surgery Center, discuss shoulder surgery with an emphasis on patient involvement in the UWTV video, "Total Shoulder Replacement: Partnership with the Patient".
Click to play
Symptoms & Diagnosis
Types of arthritis
Osteoarthritis, rheumatoid arthritis, arthritis after injury (traumatic arthritis), arthritis after previous surgery (for example, capsulorrhaphy arthropathy), chondrolysis and arthritis associated with rotator cuff disease (known as cuff tear arthropathy). Arthritis may also follow infection; this is known as septic arthritis. If the ball of the shoulder joint (humeral head) dies from lack of circulation, a condition known as avascular necrosis of the shoulder may result. Glenoid dysplasia may also be associated with arthritis.
Similar conditions
Shoulder arthritis must be distinguished from rotator cuff disease, frozen shoulder, and neck arthritis, each of which may produce similar symptoms. Rotator cuff tears usually cause pain and weakness, but stiffness is less common. Frozen shoulder is characterized by shoulder stiffness, but the X-rays are usually normal. Neck arthritis may cause shoulder pain and weakness that is worse when the head is held in certain positions.
Incidence and risk factors
While not as common as rotator cuff disease, shoulder arthritis is among the most prevalent causes of shoulder pain and loss of function. Arthritis of the shoulder joint is less common than arthritis of the hip or knee. Individuals with arthritis in one joint are more likely to get it in another joint.
Diagnosis
A physician diagnoses shoulder arthritis by reviewing the patient's history, performing a thorough physical examination of the joint and taking the proper X-rays. The examination of an arthritic shoulder reveals stiffness and roughness of the joint.
Properly taken X-rays of the shoulder (Figure 5) reveal the contour of the joint surfaces and the status of the cartilage space between them. X-rays of an arthritic shoulder (Figures 6 and 7) usually show a narrowing of the space between the ball and socket--often to the point that bone is touching bone. These x-rays show bone spurs at the bottom of the joint and reveal that the ball is not centered and has worn down the back part of the socket. These findings indicate that the normal cartilage has been destroyed. X-rays do not show the soft tissues, such as scar tissue, that may also be limiting joint motion.
Treatments
Medications
Medications may be helpful in managing arthritis. In the case of rheumatoid arthritis, specific drugs may treat the inflammation that destroys the cartilage. Some of these medications are administered by injection and others by mouth. Some individuals take anti-arthritic medications for their entire lives. These medications can be quite helpful, but there may be side effects. These medications should be taken under the close supervision of a rheumatologist or other physician experienced in their use. In other types of arthritis, anti-inflammatory drugs may lessen the pain, but do not change the course of the condition. It is important that the patient be aware of the possible side effects of these medications, including stomach irritation, kidney problems and bleeding. Injections of steroids (cortisone) or lubricants (such as hyaluronic acid) into the shoulder have not been demonstrated to have lasting benefit and carry some risk of infection.
For each medication, patients should learn:
- the risks,
- possible interactions with other drugs,
- the recommended dosage, and
- the cost.
Shoulder replacement surgery
If exercises and medication do not result in satisfactory improvement of comfort and function, shoulder joint replacement surgery may be considered. In experienced hands, this procedure can address the restricting scar tissue that frequently accompanies arthritis. It can also restore smooth, stabilizing joint surfaces when these surfaces have been damaged by arthritis.
Joint replacement surgery can improve the mechanics of the shoulder, but cannot make the joint as good as it was before the onset of arthritis. In many cases, the tendons and muscles around the shoulder have been weakened from prolonged disuse before the shoulder replacement. The scar around them needs to be removed. After the surgery, it may take months of gentle exercises before the shoulder achieves maximum improvement.
The effectiveness of the procedure depends on the health and motivation of the patient, the condition of the shoulder, and the expertise of the surgeon. When performed by an experienced surgeon, shoulder replacement arthroplasty usually provides improved shoulder comfort and function. The greatest improvements are in the ability of the patient to sleep, to perform activities of daily living, and to perform non-contact recreational activities.
Who should consider shoulder replacement surgery?
Joint replacement surgery is considered when:
- the arthritis is a major problem for the patient,
- the patient is sufficiently healthy to undergo the procedure,
- the patient understands and accepts the risks and alternatives,
- there is sufficient bone and tendon to permit the surgery, and
- the surgeon is experienced in shoulder replacement surgery.
Total shoulder replacement is most effective when the patient follows a simple exercise program after surgery. Thus, the patient's motivation and dedication are important elements of the partnership.
What happens without surgery?
In general, this surgery is elective, and can be performed whenever conditions are optimal. Sometimes the pain and stiffness from shoulder arthritis will stabilize at a level that is acceptable to the patient. In such cases the patient can delay surgery without compromising the potential for future surgery. However, in cases of rheumatoid arthritis, excessive delay may result in loss of the tendon and bone, making the surgery more difficult for the patient and for the surgeon.
Surgical options
Several types of shoulder arthroplasty are used to manage arthritis. In total shoulder arthroplasty, the surfaces of both the humeral head (ball) and the glenoid (socket) are resurfaced with metal and plastic implants. In a ream and run procedure, the humeral head is replaced as in a total shoulder, but the glenoid is reamed and allowed to heal without insertion of a plastic socket. In shoulder hemiarthroplasty, only the humeral head surface is replaced. A reverse total shoulder is used when there is arthritis and instability of the joint related to rotator cuff deficiency.
Effectiveness
In the hands of an experienced surgeon, shoulder arthroplasty can be very effective in restoring comfort and function to the shoulder of a well-motivated patient. The greatest benefits are often the ability to sleep on the affected shoulder and the ability to perform usual activities of daily living. As long as the shoulder is cared for properly and subsequent injuries are avoided, the benefit can last for decades.
Urgency
Shoulder arthroplasty for arthritis is an elective procedure that can be scheduled when circumstances are optimal. It is not an urgent procedure. The patient has plenty of time to become informed and to select and experienced surgeon.
Risks
The risks of total shoulder surgery include but are not limited to the following: infection, injury to nerves and blood vessels, fracture, stiffness or instability of the joint, loosening or wear of the artificial parts, failure of the rotator cuff, pain, and the need for additional surgeries. There are also risks to anesthesia and blood transfusion (although transfusions are not always necessary). An experienced shoulder joint replacement team will use special techniques to minimize these risks, but cannot totally eliminate them.
Managing risk
Many of the risks of shoulder arthroplasty surgery can be effectively managed if they are promptly identified and treated. Infections may require a "wash out" in the operating room--occasionally removal of the artificial components is necessary. Blood vessel or nerve injury may require repair. Fracture may require surgical fixation. Stiffness or instability may require exercises or additional surgery. Loosening or wear of the components may require surgical revision. If the patient has questions or concerns about the course after surgery, the surgeon should be informed as soon as possible.
Preparation
Total shoulder joint replacement surgery is considered for healthy and motivated individuals in whom arthritis interferes with shoulder function.
Successful shoulder replacement depends on a partnership between the patient and the experienced shoulder surgeon. Patients should optimize their health so that they will be in the best possible condition for this procedure. Smoking should be stopped a month before surgery and not resumed for at least three months afterwards. Any heart, lung, kidney, bladder, tooth, or gum problems should be managed before surgery. Any infection may be a reason to delay the operation. The shoulder surgeon needs to be aware of all health issues, including allergies and the non-prescription and prescription medications being taken. Some of these may need to be modified or stopped. For instance, aspirin and anti-inflammatory medication may affect the way the blood clots. Since blood transfusion may be necessary.
The skin of the shoulder and arm must be clean and free from sores and scratches.
Before surgery, patients should consider the limitations, alternatives and risks of surgery. Patients should also recognize that the result of surgery depends in large part on their efforts in rehabilitation after surgery.
The patient needs to plan on being less functional than usual for six to twelve weeks after the procedure. Driving, shopping and performing usual work or chores may be difficult during this time. Plans for necessary assistance need to be made before surgery. For individuals who live alone or those without readily available help, arrangements for home help should be made well in advance.
Timing
Shoulder replacement arthroplasty can be delayed until the time that is best for the patient's overall well-being. However, in cases of rheumatoid or other types of inflammatory arthritis, excessive delays can result in the loss of bone and tendon tissue. These losses can compromise the quality of the surgery and its result.
Costs
The surgeon's office should provide a reasonable estimate of:
- the surgeon's fee, and
- the hospital fee.
Surgical team
Shoulder replacement arthroplasty is a technically demanding procedure that should be performed by an experienced surgeon in a medical center accustomed to performing shoulder joint replacements at least several times a month. Patients should inquire as to the number of shoulder arthroplasty procedures that the surgeon performs each year and the number of these procedures performed in the medical center each year.
Finding an experienced surgeon
Because less than twenty thousand of these procedures are performed in the United States each year, it is unlikely that every community has an experienced shoulder arthroplasty surgeon who performs many of these procedures each year..
Facilities
Shoulder replacement arthroplasty is usually performed in a major medical center that performs these procedures on a regular basis. These centers have surgical teams and facilities specially designed for this type of surgery. They also have nurses and therapists who are accustomed to assisting patients in their recover from shoulder replacement surgery.
Technical details
Shoulder replacement surgery is a highly technical procedure; each step plays a critical role in the outcome.
After the anesthetic has been administered and the shoulder is prepared, an incision is made across the front of the shoulder from the middle of the collarbone to the middle of the arm bone. This incision allows access to the joint without damaging the important deltoid or pectoralis muscles that are responsible for a significant portion of the shoulder's power.
The muscles and other tissues near the shoulder are mobilized by removing any scar tissue that may restrict their motion. The tendon of the subscapularis muscle is cut to gain access to the joint and released circumferentially (a 360-degree release) to restore its length and mobility. The arthritic humeral head (ball of the joint) is removed. The bone spurs are removed to prepare the bone for the humeral prosthesis. The humeral component is made of metal and is usually press fit, but sometimes cemented, into the shaft of the bone of the humerus.
If the glenoid is affected, but conditions do not favor the insertion of a glenoid component, a non-prosthetic glenoid arthroplasty may be performed along with a humeral hemiarthroplasty. In this procedure, the glenoid shape and orientation are corrected, but a glenoid prosthesis is not inserted. The reshaping of the socket using a spherical reamer is shown in the figure. The prosthetic ball of the humeral component articulates with the reshaped bony socket of the glenoid. This procedure may be selected when the patient is interested in performing heavy activities that might endanger the fixation of a polyethylene glenoid component.
In a total shoulder joint replacement, the glenoid bone is shaped and oriented as in the non-prosthetic glenoid arthroplasty and then covered with a polyethylene glenoid component, as seen in the figure. A small amount of bone cement is used to hold the artificial glenoid socket in place.
At the conclusion of any of these procedures, the subscapularis tendon is securely repaired to the bone. This repair requires protection from active use for at least 6 weeks while it is healing.
Anesthetic
Shoulder joint replacement surgery is performed under a general anesthetic.
Length of shoulder replacement surgery
The procedure usually takes approximately two hours, however the preoperative preparation and the postoperative recovery may add several hours to this time. Patients often spend two hours in the recovery room and two to four days in the hospital after surgery.
Pain and pain management
Recovery of comfort and function after shoulder arthroplasty continues for the first year after surgery. The rehabilitation is carried out largely by the patient under the supervision of the surgeon.
Shoulder replacement arthroplasty is a major surgical procedure that involves cutting of skin, tendons and bone. The pain from this surgery is managed by the anesthetic and by pain medications. Immediately after surgery, strong medications (such as morphine or Demerol) are often given by injection. Within a day or so, oral pain medications (such as hydrocodone or Tylenol with codeine) are usually sufficient.
Use of medications
Initially pain medication is usually administered intravenously or intramuscularly. Sometimes patient controlled analgesia (PCA) is used to allow the patient to administer the medication as it is needed. Hydrocodone or Tylenol with codeine are taken by mouth. Intravenous pain medications are usually needed only for the first day or two after the procedure. Oral pain medications are usually needed only for the first two weeks after the procedure.
Effectiveness of medications
Pain medications can be very powerful and effective. Their proper use lies in the balancing of their pain relieving effect and their other, less desirable effects. Good pain control is an important part of the postoperative management.
Important side effects
Pain medications can cause drowsiness, slowness of breathing, difficulties in emptying the bladder and bowel, nausea, vomiting and allergic reactions. Patients who have taken substantial narcotic medications in the recent past may find that usual doses of pain medication are less effective. For some patients, balancing the benefit and the side effects of pain medication is challenging. Patients should notify their surgeon if they have had previous difficulties with pain medication or pain control.